- What is it?
- Diagnosis
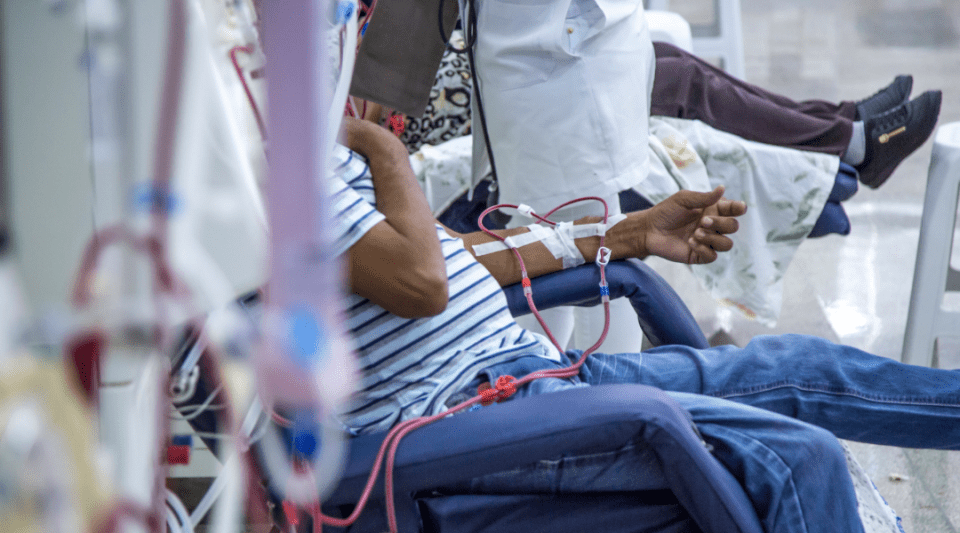
- Treatment
- Type 1 diabetes
- Type 2 Diabetes
- Gestational Diabetes
- Disease evolution
- Living with the disease
- Research lines
- Frequently Asked Questions
- Diabetes at the Clínic
- Gestational Diabetes at the Clínic
- Research at the Clínic
- Teaching and Training at the Clínic
- Team and structure
What is Type 1 Diabetes?
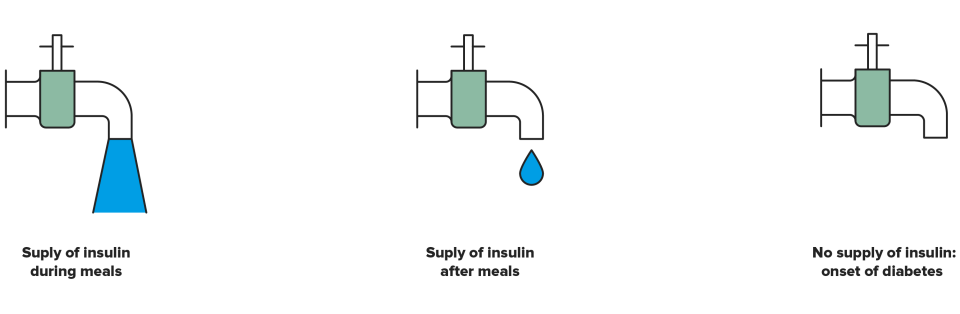
The tap metaphor has proven very useful when it comes to explaining how the body supplies insulin. The patient is asked to consider a tap which controls the flow of insulin rather than water. This biological insulin tap is always open, dripping constantly because we all require a continuous, round-the-clock supply of insulin. But we do not need the same amount at all times; in which situations does the insulin tap open more? During meals. Afterwards, the tap returns to the drip mode and never fully closes because the body still requires some insulin. So what happens if the tap closes completely? This is the onset of diabetes type 1.
Type 1 diabetes represents between 5% and 10% of all cases of diabetes. It should be mentioned that it is one of the most common chronic diseases in childhood. The onset occurs in children and young adults, hence it is also known as juvenile diabetes. The most common age of onset is between 11 and 14 years. Although less frequent, type 1 diabetes may also develop from the age of 40 onwards. Information on the characteristics of treatments used in under 18s can be found on the Hospital Sant Joan de Déu website, which is the paediatric hospital at our health centre.
Despite our knowledge of many of the mechanisms involved in type 1 diabetes, of which genetic and environmental factors play an important role, the actual cause is still unknown. While the overall risk of developing type 1 diabetes mellitus is low (1 in every 10,000 people per year), the following individuals present a higher risk:

Siblings of people with type 1 diabetes.

Children whose mother or father has type 1 diabetes. Additionally, if both the mother and father have diabetes then the risk is even greater.
Early symptoms that cause people to visit their doctor and which are associated with high sugar levels are:

Frequent urge to urinate (polyuria).

Increased thirst (polydipsia).

Increased hunger (polyphagia).

Weight loss.

Other less common symptoms are tiredness, leg cramps and sleepiness.
All people with type 1 diabetes know that they have this disease. However they can be diagnosed, because the symptoms are very clear and they should ask the doctor, which can make the diagnosis and start treatment.
Diabetes is diagnosed by means of a blood test that determines a person’s blood sugar (glucose) levels. Normal blood glucose values range between 70 and 100mg/dL.
This test analyses whether the analytical indicators are:
- After fasting: equal to or higher than 126 mg/dL, in two measurements.
- At any time of the day: equal to or greater than 200 mg/dL accompanied by characteristic symptoms, such as an increased need to urinate or excessive thirst.
- Glycated hemoglobin (HbA1c): equal to or higher than 6.5%.
The main markers of autoimmune destruction that can be identified in a blood analysis are:
- Anti-islet cell antibodies (ICA)
- Anti-insulin antibodies (AIA)
- Antibodies against tyrosine-phosphatase or insulinoma-associated protein-2 (IA-2)
- Glutamic acid decarboxylase antibodies (GADA)
People with type 1 diabetes have to inject insulin, measure their capillary blood glucose before meals and follow a balanced eating plan in order to live.
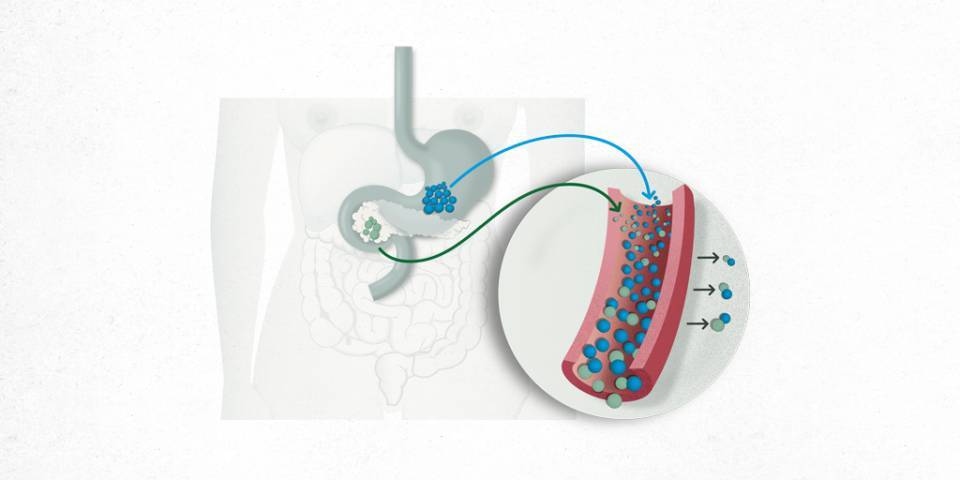
Insulin is a hormone produced by the pancreas that helps the body make use of glucose derived from food. This is the insulin produced naturally by the body, but the type administered to patients is different.
There are two treatment systems involving insulin:
- Multi-dose insulin treatments: these involve administering:
- Rapid-acting insulin: to be administered before meals (between 3 – 4 times per day).
- Long-acting insulin: taken once or twice a day to cover the body’s background (basal) insulin requirements.
- Insulin infusion pumps: consist of administering insulin by means of continuous, subcutaneous insulin infusion (insulin pump).
There are several types of insulin available. They are classified according to the time they take to act or the time until the onset of action and the duration of the effect. Based on your needs, you will be advised to inject:
- Ultra-rapid (rapid-acting insulin analogues)
- Normal insulin
- Intermediate-acting insulin (NPH and NPL)
- Long-acting (long-acting insulin analogues)
- Premixed rapid- and intermediate-acting insulin. The first number corresponds to the percentage of rapid insulin and the second is the percentage of intermediate insulin.
- Premixed ultra-rapid- and intermediate-acting insulin in different proportions.
There are several brands of each type of insulin available and also different administration devices. Your healthcare team will instruct you about the type of insulin, brand, number of units you should inject, recommended time between injecting and starting your meal and the most preferable injection areas in each case.
Insulin can only be administered via an injection; however, research is being carried out into new administration routes. The type of instrument used is recommended in function of each patient and their particular situation:
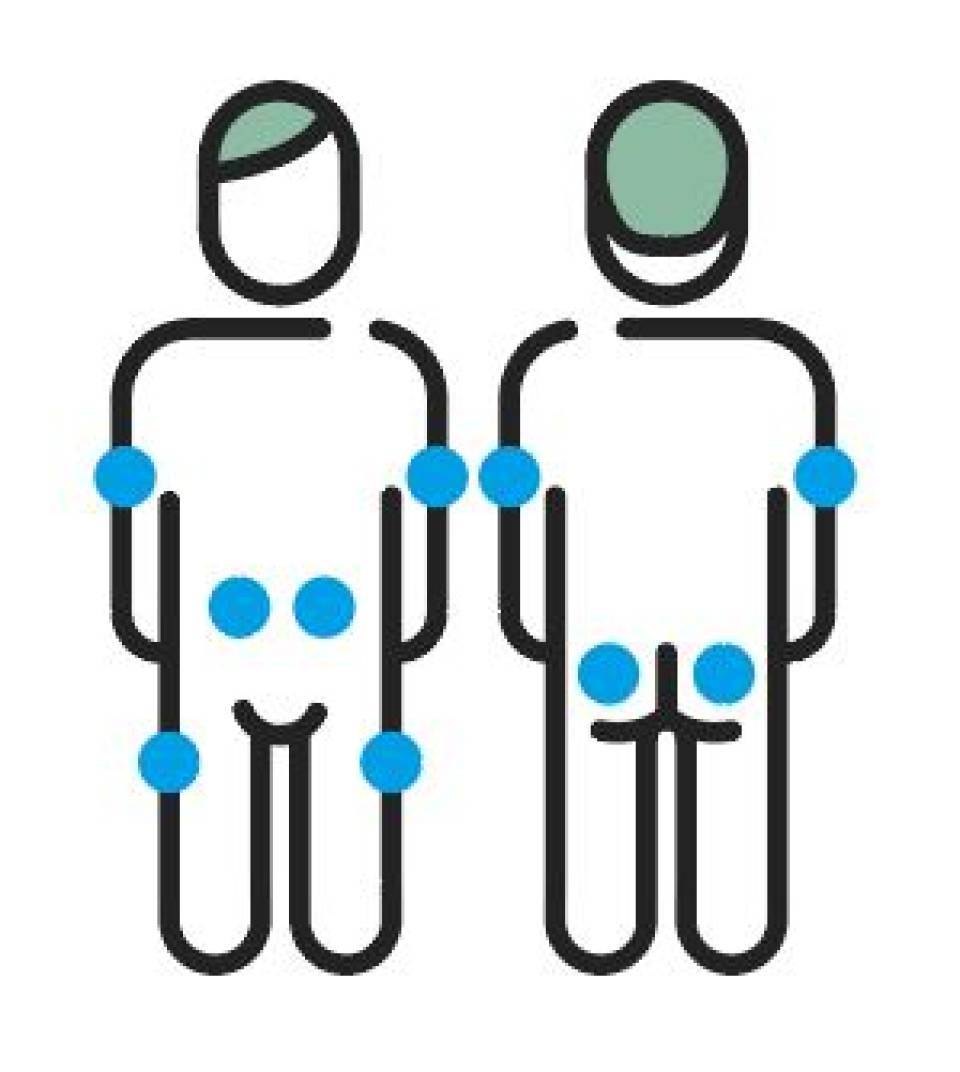
Insulin is injected into subcutaneous tissue. It can be injected into the areas indicated below. You need to alternate the injection area so that the years of injections do not cause hypertrophy (localised volume increase in tissue) or hardened skin, which can prevent the insulin from working correctly. Injection site areas are:
- Arms. Insulin should be injected into the external area of the upper lateral portion of your arm, but ensure it is at least four finger-widths away from your shoulder.
- Thighs. Insulin should be injected into the upper lateral external portion of your thighs.
- Abdomen. You can inject into the abdomen, but ensure it is at least two finger-widths away from your naval.
- Buttocks. Subcutaneous tissue in this area is abundant in both adults and children and so injections are very safe. The injection must be made at least 10 cm below the height of the hip bone.

Injection

Single-use pens

Insulin pumps
Note that rapid- or long-acting insulin analogues are absorbed at the same rate regardless of the injection area. It is a good idea to use the same area (but changing the specific site) at the same time of day. In any case, recommendations are to inject rapid-acting insulin into the abdomen and upper arms, whilst long-acting insulin or long-acting analogues should be injected into the thighs or buttocks for correct rotation.
In the case of human insulins, absorption can vary slightly in function of the area where the insulin is injected. Insulin is absorbed most rapidly when injected into the abdomen, followed by the upper arms, thighs and buttocks. Therefore, rapid-acting insulin should be injected into the abdomen and long-acting insulin is best injected into the legs and buttocks.
All of the needles are designed for single-use, but despite recommendations to replace them after each injection, they are often reused more than once. The patient’s age and number of injections per day must always be taken into account. Patients should never reuse the same needle more than three times. Individuals who reuse needles have a 30% greater risk of developing a hypertrophy.
Needles of varying lengths are currently available on the Spanish market. They are:
- For pens: 4, 5, 6, 8 mm
- For syringes: 8 mm
An evaluation of needle length, injection area and administration technique is a key factor when ensuring correct subcutaneous absorption of the insulin. The thickness of the subcutaneous layer may vary according to the injection area (abdomen, thigh, buttocks or upper arm), patient sex, body mass index, body shape and distribution of abdominal fat.
Different studies have demonstrated that shorter needles, measuring 4 or 5 mm, are suitable for everyone, even if they are obese.
Each patient must customise their insulin administration technique in terms of whether or not they pinch a fold of skin or inject at an angle of 90° or 45° to obtain correct absorption.
- Lipohypertrophy. This occurs when lumps of subcutaneous cellular tissue appear due to repeated insulin injections in the same area over a long period of time. Factors predisposing the appearance of lipohypertrophy are: the insulin injected, repeated microtrauma in the injection area and the reuse of needles. The prevalence is around 30–51%. Lipohypertrophy has negative repercussions on metabolic control given that it causes erratic insulin absorption and also requires larger doses of insulin. Therefore it is important to plan appropriate and systematic rotation of the injection areas and avoid reusing needles from the outset.
- Lipoatrophy. This is a loss of subcutaneous tissue in injection areas. It occurs due to an immunological reaction produced by the actual insulin. Its prevalence is much lower since the introduction of new insulins.
- Infections. These are uncommon when using pens or syringes. A good level of hygiene is enough to prevent infections. Nevertheless, they still represent a significant risk in people who use continuous insulin infusion systems. In such cases patients are advised to maximise hygiene measures and use antiseptic agents in the cannula insertion area.
Types of insulin administered via cartridges (pens) have a concentration of 1/100 everywhere around the world, but insulin in vials may not have the same concentration.
A vial or pen of insulin is stable at room temperature for one month, so long as the temperature does not exceed 30 °C. If this happens, then it should be stored in a cork box or an isothermal bag. Spare supplies of insulin must be stored in the refrigerator at temperatures of 2–8 °C.
In general, everybody, with or without diabetes, should follow a healthy, balanced and varied eating plan. Eating plans should be customised according to the patient’s age, level of activity, timetable, body weight and personal preferences.
Familiarity with this ratio is important because it means you can be flexible with the portion of carbohydrates in meals and adjust the insulin accordingly.
What is the ratio?
The ratio corresponds to the amount of insulin required to cover one portion of carbohydrates.
How is it calculated?
A good method of calculating the ratio is to eat the same amount of carbohydrates and then check whether your sugar levels are less than 180 mg/dL two hours after eating (postprandial). Once you know this value, divide the units of insulin for one meal by the number of carbohydrate portions to obtain the ratio.
EXAMPLE: We first establish that eating 6 portions of carbohydrates requires 12 units of insulin. 12 units / 6 por. = 2 units/por.
Therefore, in this example, the patient must inject 2 units of insulin for each portion of carbohydrates they intend to eat. It is important that people with diabetes are aware of the amounts of different foods they eat regularly and how much is equivalent to 1 portion of carbohydrates so they can quantify each meal. They should also know the equivalents in order to be able to make exchanges.
Physical activity adapted to the abilities of each person and practised regularly can contribute very positively to achieving good control over diabetes, reducing cardiovascular risk factors (obesity, high cholesterol, etc.) and improving one’s sense of mental and physical well-being. In the case of type 1 diabetes, exercise is recommendable simply to maintain a good physical condition. Some tips concerning exercise:
|
Before |
During |
After |
|
Check your capillary blood glucose level and act according to the plans you discussed with your healthcare team. |
Always carry fast-absorbing carbohydrates with you to correct any episodes of hypoglycaemia. |
Measure your capillary blood glucose level |
|
If you take insulin before the exercise, you can: |
If exercising with other people, then it is a good idea to let them know what to do if you suffer an episode of severe hypoglycaemia. |
In the case of extended exercise, decrease subsequent dose of insulin or increase your intake of carbohydrate-rich foods. |
|
|
Stay well hydrated |
|
Type 1 diabetes and sport. For children, adolescents and young adults. Serafín Murillo. 2012
Collaboration between people with diabetes and their families and healthcare teams is essential for optimizing the treatment and, at the same time, for integrating it into their day-to-day life in terms of regular eating habits, timetables and physical activity.
Therapeutic education in diabetes is a learning process that provides the knowledge and skills required by people with diabetes and their families so they may actively take part in everyday treatment decisions.
Continuous subcutaneous insulin infusion (CSII) systems provide a constant infusion of insulin within the subcutaneous layer. The insulin is infused via a catheter inserted under the patient’s skin. The catheter must be changed every 3 days to avoid infections and/or saturating the subcutaneous tissue. Infusion pumps help achieve better control over your diabetes. There are 6 and 9 mm pump cannulae available for injecting at a 90° angle, and 13 and 17 mm cannulae for injecting at an angle of 45°.
The insulin is supplied by means of two totally distinct systems:
- Basal insulin. The pump administers insulin continuously, 24 hours a day and according to a programmed schedule. A certain amount of insulin is injected every hour, or time block, and can be set according to the patient’s needs at different times of the day. It is equivalent to the long-acting insulin patients administer once or twice a day using a pen.
- Bolus insulin. This insulin is administered with each meal or to correct an episode of hyperglycaemia. It is equivalent to the rapid-acting insulin patients inject before meals.
Basic concepts associated with insulin pump therapy.
- Meal bolus: insulin administered with each meal.
- Correction bolus: an additional and occasional administration of insulin taken according to capillary blood glucose levels and the insulin sensitivity factor.
- Bolus calculator or bolus Wizard: a feature included with infusion pumps that assists decision-making when administering different types of bolus.
- Insulin sensitivity factor: the decrease in blood glucose (in mg/dL) produced by 1 extra unit of insulin when taking a correction bolus. For example, if your insulin sensitivity factor is 50 mg/dL, then one extra unit will reduce your blood glucose by 50 mg/dL. Hence, if your level is 200 mg/dL before eating and the target is 150 mg/dL, you need to take a correction bolus of one extra unit.
- Basal insulin: the insulin the pump administers continuously, 24 hours a day, and according to a programmed schedule.
- Temporary basal insulin: insulin that can be temporarily increased or decreased above the programmed basal rate.
- Insulin to carbohydrate ratio: amount of insulin required for 1 portion of carbohydrates.
Recommendations for preventing and treating injection site irritations and/or infections for patients with insulin pumps
- Ensure maximum hygiene measures when inserting the catheter.
- Change the needle every 3 days, or sometimes even every 2 days.
- Make daily checks for any anomalies, redness, irritation or pain at the injection site. If after these preventive measures these symptoms still appear:
- Change the catheter and injection area.
- Get in touch with your healthcare team for a possible treatment. Remember that it could cause hyperglycaemia even if you have done everything correctly.
Recommendations for preventing and/or treating hypoglycaemia in patients wearing insulin pumps
To prevent your blood sugar level from falling below 70 mg/dL (hypoglycaemia), you have to measure your level according to your healthcare team’s instructions, at least 3 or 4 times a day, and ensure that it is:
- Not less than 80 mg/dL before eating.
- Not less than 120–140 mg/dL before going to sleep, before driving and at 3 a.m. If you have a history of severe or very frequent episodes of hypoglycaemia, then these limits could be higher.
- If you do more physical exercise than normal, then you must eat more carbohydrates (carbs) or use the temporary basal insulin bolus.
- If you wish to eat fewer portions of carbs, then you need to adjust the insulin bolus to the meal.
Recommendations for family and friends when faced with a severe episode of hypoglycaemia in patients wearing insulin pumps
- You should not attempt to give someone who has fainted anything by mouth.
- They must be injected with GlucaGen® HypoKit 1 mg glucagon (which must be stored in a refrigerator).
- The pump must be disconnected or the catheter cut at the nearest possible point to the injection site.
- When the person comes round, you should give them a fruit juice or equivalent and contact their medical team.
Recommendations for preventing and/or treating hyperglycaemia in patients wearing insulin pumps
- Monitor and/or detect anything obstructing insulin infusion early on: air bubble, a blocked catheter/needle, etc.
- Control the number of portions of carbohydrates in meals. If you wish to eat more portions, then you will have to adjust the insulin bolus.
- You will have to use the temporary basal insulin if you carry out less physical exercise.
- Remember that an infection could cause severe hyperglycaemia even though you have done everything correctly.
If, despite all the preventive measures, you still observe levels of above 250 mg/dL before meals or midnight
- Then you must always perform a ketone in urine test. If the ketone test is negative, you should administer a correction bolus of extra insulin according to your sensitivity factor or use the bolus calculation feature on your pump.
- You must then check whether the infusion system is working correctly. If you notice any bubbles, you need to purge them or change the needle.
- If after 1 or 2 hours your sugar levels are still above 250 mg/dL, or have not dropped with respect to previous measurements, then you must inject rapid-acting insulin, or an analogue, with a pen. Do not administer a second correction bolus using the pump if the first one did not produce the desired effect. You must subsequently change the infusion set.
- If after 1 or 2 hours your blood sugar levels remain high, you give a positive ketone test and have followed the above indications, then you should contact your healthcare team.
Substantiated information by:





Published: 20 February 2018
Updated: 24 November 2021
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox