- What is it?
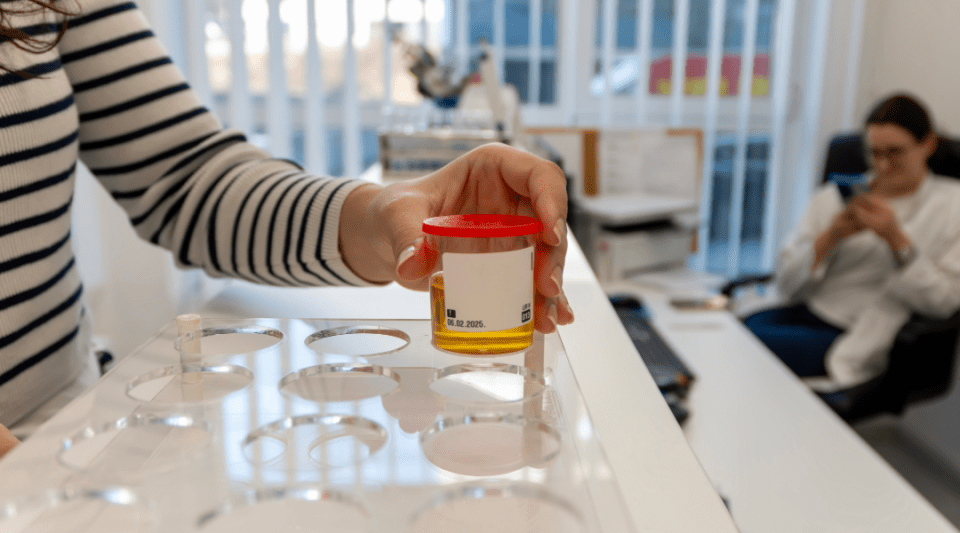
- Diagnosis
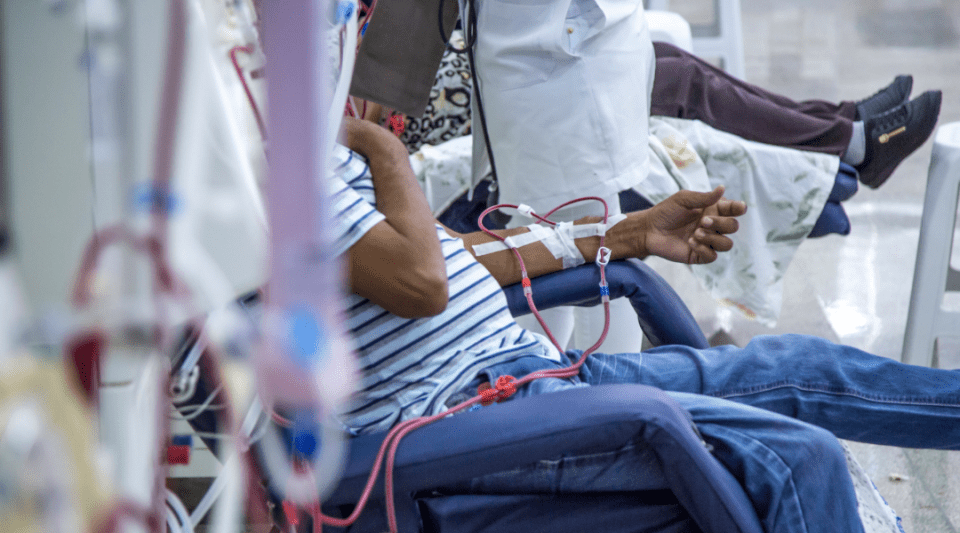
- Treatment
- Type 1 diabetes
- Type 2 Diabetes
- Gestational Diabetes
- Disease evolution
- Living with the disease
- Research lines
- Frequently Asked Questions
- Diabetes at the Clínic
- Gestational Diabetes at the Clínic
- Research at the Clínic
- Teaching and Training at the Clínic
- Team and structure
Diabetes evolution
Diabetes is a chronic disease and does not have a cure, except for the case of gestational diabetes which usually disappears after childbirth. Treatments have improved a great deal in recent years and research continues to discover preventive strategies and new treatments.
Hypoglycaemia occurs when your blood glucose level falls below 70 mg/dL. All patients treated with insulin or some oral antidiabetic drugs, can experience an episode of hypoglycaemia.
The most common symptoms are:

Tremors, sweating, paleness, palpitations, feeling hungry, dizziness (known as adrenergic symptoms).

Altered speech, blurred vision, lack of coordination (called neuroglycopenic symptoms).

Some people do not notice any changes when they have blood sugar levels below 70 mg/dL. This is known as undetected hypoglycaemia. Patients who experience episodes of undetected hypoglycaemia must maximise preventive measures more than ever to ensure their safety.
Hypoglycaemia is caused by:

Not eating or eating a meal later than usual.

Doing more exercise than usual.

Injecting more insulin than usual in relation to your carbohydrate intake.

Drinking a significant amount of alcohol can also provoke the onset of hypoglycaemia.
In case of hypoglycaemia, you must eat or drink ONE of the following options:

1 glass (200 mL) of fruit juice, or

1 glass of milk and 1 sachet of sugar, or

2 sachets of sugar, or

1 glass or ½ can of a soft drink (that is not sugar-free or light).
Severe hypoglycaemia
A drop in sugar levels that leads to partial or total loss of consciousness. A person with severe hypoglycaemia must be helped by somebody else.
Advice for family members and friends
- If the person has not lost consciousness, try to give them a glass of fruit juice or a sugared soft drink (1 glass). They must not be lying down at the time; you must try to give them the drink while they are sat up.
- If they are unconscious or speak incoherently, then you should not give them anything by mouth. In such cases, you should inject them with glucagon (GlucaGen® HypoKit 1 mg). Once ready, inject the glucagon in any area where they normally administer insulin to raise their blood sugar level and help them recover consciousness. Nasal glucagon (single dose of 3mg) can also be administered.
- Once the patient has regained consciousness, give them fruit juice or something similar and get in touch with their healthcare team.
- If you do not have any glucagon, call emergency services (112).
Hyperglycaemia is an excessively high amount of sugar in the blood. All diabetes patients, regardless of whether their treatment is with insulin, tablets or through diet and exercise, can suffer episodes of hyperglycaemia.
Some people do not notice any difference. While others may be thirsty, need to urinate more and, occasionally, may even lose weight despite feeling hungrier and eating more. The best way of finding out if your sugar level is high is to measure your capillary blood glucose level.
Hyperglycaemia is caused by:

Eating foods with a high sugar content: soft drinks, bakery products, cakes, ice-creams, chocolate.

Eating more fruit, grains and milk products than usual.

Exercising less than usual.

Forgetting to inject insulin.

Infections: a cold, a boil, etc., especially if the patient has a fever. An infection can be a cause of hyperglycaemia even when all the other signs are correct.
An infectious process may rapidly result in an uncontrolled metabolism. Hormone and sugar levels tend to increase during infections and so patients must take the following into account:

Even if you eat fewer carbohydrates, you will probably still need to take rapid-acting insulin to correct high sugar levels.

Hydrate yourself correctly, particularly if you have gastroenteritis, to prevent dehydration.

Increase the frequency of capillary blood glucose and ketones in urine or blood tests, if necessary.

Treat the infection causing the hyperglycaemia.
In case of doubt, high ketone levels or if you experience nausea and vomiting, you should get in contact with your healthcare team promptly or go to the nearest hospital.
In case of hyperglycaemia

Drink more water than usual, even if you are not thirsty, to prevent dehydration.

Carry out more capillary blood sugar tests and check your ketones in urine level.

Never stop taking your insulin injections at the agreed times. You may need to increase the dose if the hyperglycaemia lasts for more than two hours.

If you are not hungry, you may stop eating salads and/or vegetables, meat, fish, etc., but you must always ensure the same amount of grains, fruit and milk products, and adapt their preparation, e.g., eating grains in soups, semolina, or drinking fruit juices.
Visit your doctor if...
- You feel unwell,
- your capillary blood sugar level exceeds the maximum value recommended by your healthcare team, or
- your capillary blood sugar is greater than 250–300 mg/dL and the ketones in urine test is positive.
Diabetic ketoacidosis is an acute imbalance typically associated with type 1 diabetes, and also, but much less frequently, with type 2 diabetes. It is characterised by excessively high ketone levels in the blood. These high blood ketone levels are due to an insulin deficit or increased insulin requirements (e.g., because of an infection) which means the body cannot use glucose as an energy source and must use fats instead. This phenomenon results in an excess of ketone bodies in the blood (by-products released when fats are used as an energy source). The presence of ketone bodies in the blood can reduce blood pH; this may evolve into a life-threatening situation that requires hospitalisation.

What will I notice? Excessive ketone levels sustained throughout the day may cause gastric distress, nausea, vomiting and even breathing difficulties. You may notice that your breath tastes of apple.

What should I do? Contact your healthcare team as soon as possible.
Hyperosmolar syndrome is an acute imbalance that occurs in patients with type 2 diabetes. It is characterised by extremely high blood sugar levels, but without the presence of ketones.

Hyperosmolar syndrome can produce symptoms such as: excessive thirst and/or need to urinate, weakness, nausea, weight loss, dry mouth and tongue, convulsions, confusion and coma.

What should I do? Contact your healthcare team as soon as possible. If you do not act, then there is a risk you could fall into a diabetic coma.
The majority of chronic complications are usually the result of a vascular problem. Vascular problems occur when large blood vessels become blocked (obstructed) or when smaller vessels are damaged, as in the case of the arteries in the eye’s retina and those found in the kidneys.
In the long-term, diabetes can affect: the eyes (diabetic retinopathy), the kidneys (chronic kidney failure), the heart (cardiopathie) or the feet (diabetic foot).
Chronic complications have diminished in recent years due to improved treatments that have provided the opportunity to obtain greater control over hyperglycaemia and other risk factors.

Maintain good control over your diabetes.

Prevent or reduce cardiovascular risk factors. Cardiovascular risk is the risk of developing a heart (angina pectoris or infarction) or brain condition (stroke) during a given period of time, generally the next 5 to 10 years. The habits or behaviours that increase this risk, which are what we call cardiovascular risk factors, are: cholesterol, high blood pressure, being overweight and obesity, smoking tobacco, diabetes and stress.

Once patients have adapted to the treatment, and depending on each case and situation, check-ups with the healthcare team are usually held every 3 or 6 months. Some studies have provided conclusive evidence that good metabolic control prevents or delays the onset of future complications associated with diabetes and therefore improves the quality of life.
As the years pass, people with diabetes can experience a loss of nerve sensitivity (neuropathy), particularly in the lower limbs, and may also notice tingling, cramps, or an inability to feel cold, heat or pain. They may also have vascular problems (obstructed vessels) meaning their feet are prone to a greater risk of suffering injuries and difficult-to-treat infections.
People with the following characteristics present a greater risk of developing these problems:
- elderly,
- long-term presence of diabetes,
- poorly controlled diabetes,
- smokers,
- high cholesterol,
- high blood pressure,
- flexibility problems and
- vision problems.
Preventing and treating diabetic foot
Not everybody with diabetes has the same risk of suffering from diabetic foot. Ask your healthcare team whether you have a low or high risk of diabetic foot so you can follow the appropriate recommendations for your situation:
Recommendations for people with a low risk:
Hygienic care for your feet: wipe dry, hydrate, cut toenails straight, wear breathable tights and socks that do not narrow, and wear appropriate footwear – good hygiene recommendations for everybody, with or without diabetes.
Recommendations for people with a high risk:
- Control the water temperature (warm water or adjusted to a temperature of 36 or 37 °C using a thermometer).
- Maximise hygiene with daily drying and hydration.
- Avoid heat sources (do not place your feet in front of the fire, do not use hot water bottles, etc.).
- Use footwear fitted to the shape of your feet, made from soft leather that can adapt to any deformities. Shoes must be lined and have minimal stitching or decoration to avoid injuring your feet.
- Inspect your feet daily for any small scratches; use a mirror if you have difficulties due to low flexibility.
- Do not use a file to remove hard skin. Ask either a chiropodist or somebody else to cut your toenails, particularly if you have flexibility and/or vision problems.
- Always discuss any small wounds with your doctor, even if they are painless.
- Check for loss of sensitivity (neuropathy).
Substantiated information by:





Published: 20 February 2018
Updated: 24 November 2021
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox