- What is it?
- Diagnosis
- Treatment
- Type 1 diabetes
- Type 2 Diabetes
- Gestational Diabetes
- Disease evolution
- Living with the disease
- Research lines
- Frequently Asked Questions
-
The disease at the Clínic
- Team and structure
What is Type 2 Diabetes?
Type 2 diabetes is a disease characterised by an increase in blood glucose levels derived from the body’s inability to produce or use its own insulin correctly. Type 2 diabetes mellitus develops in adulthood and so it is sometimes called elderly diabetes. It is the most common form of diabetes (80–90% of all cases).
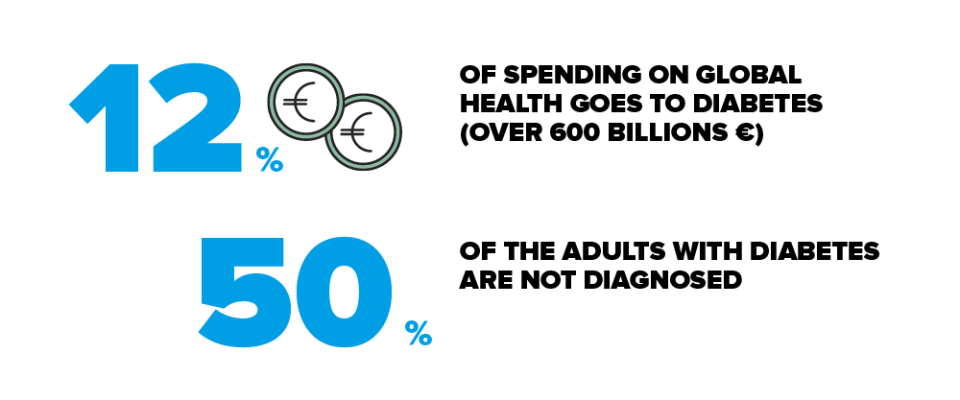
Diabetes affects millions of people around the world. The Di@bet.es study has shown that diabetes affects 13.8% of the Spanish population (i.e., its prevalence). In other words, 14 out of every 100 people have diabetes. This figure increases with age and it is more common in men than women. Consequently, 20 in every 100 people aged 60–75 years have type 2 diabetes.
Type 2 diabetes (T2D) presents a clear social gradient; people with no education or primary education are twice as likely to develop diabetes as those with a university education, and this trend is the same in both men and women.
One of the significant problems concerning type 2 diabetes is half of all sufferers are unaware of their condition because they do not present any symptoms in the early stages of the disease. It can only be diagnosed by means of a blood glucose analysis. That is why many people find out they have T2D by chance, while undergoing a routine analysis for another reason. Individuals with very high glucose levels may notice symptoms such as increased thirst, increased urge to urinate and even weight loss.
The main causes of type 2 diabetis in genetically predisposed people are obesity and a sedentary life.
They are at greater risk of developing type 2 diabetes with:

Genetic factors. A family history of diabetes and cardiovascular disease.

Sedentary habits

High cholesterol levels (hypercholesterolemia).

Gestational diabetes. It's a type of diabetes that occurs in 12% of all pregnancies in women with no prior history of diabetes, or women who have had a baby with a birth weight of 4 kg or more.

Oral glucose intolerance. These patients present higher than normal blood glucose levels, but they are not high enough to be classified as diabetic. There are two situations considered to be risk factors: if the test result is positive (values ranging between 140 and 199 mg/dL) after swallowing 75 g of glucose; or, if blood glucose levels are high (above 100 mg/dL, but less than 126 mg/dL) after eight hours of fasting.
In every 100 adults, there are around 25–30 individuals with a carbohydrate metabolism disorder (diabetes, whether diagnosed or undiagnosed, glucose intolerance or impaired fasting glucose).
In contrast to type 1 diabetes, people with a high risk of developing type 2 diabetes mellitus can prevent and/or delay the onset if they:

Maintain a correct body weight by following a healthy eating plan.

Practise regular physical activity (minimum of 150 minutes per week).
Most people are diagnosed with type 2 diabetes by chance while carrying out routine analyses for other reasons (company check-ups, gynaecological tests, etc.). The disease is present but it has not yet produced any symptoms. The early symptoms that induce patients to visit their doctor and which are associated with high sugar levels are:

Frequent urge to urinate (polyuria).

Increased thirst (polydipsia).

Increased hunger (polyphagia).

Weight loss.

Other less common symptoms are tiredness, leg cramps and sleepiness.
Type 2 diabetes mellitus is the most common kind, representing roughly 80–90% of all cases, and its onset can be prevented or delayed in the large majority of people. Studies have demonstrated that the risk factors for developing this type of diabetes are, on the one hand, the so-called non-modifiable factors, which are age and genetic predisposition, while on the other hand are the modifiable ones, which are overweight, obesity and a sedentary lifestyle.
If you would like to know your risk of developing type 2 diabetes in the next 10 years, then you can find out by completing the FINDRISK test. Based on your score in this questionnaire, you can identify your degree of risk and which measures to adopt.
This test takes these parameters into account:

Age. The risk of developing type 2 diabetes is greater in people aged over 45; notwithstanding, cases of type 2 diabetes in obese and sedentary children and adolescents have recently been described.

Body mass index (BMI). The BMI is a parameter that relates a person’s weight to their height and helps identify whether they are underweight, normal, overweight or obese. Overweight and obesity are risk factors for developing type 2 diabetes. The BMI is not applicable in the case of children, pregnant women, the very elderly and people with a high muscle mass, such as professional sportsmen and women.

Waist circumference. The circumference at the waist is an indicator of obesity. In combination with the BMI, it helps determine the risk of cardiovascular disease and type 2 diabetes mellitus. The risk is considered high if the measurement is greater than 102 cm in men and 88 cm in women.

Physical activity. A sedentary lifestyle, both in adults and children, is another risk factor related to the development of type 2 diabetes. Recommendations are to perform regular physical activity, such as 30 minutes walking per day.

Eat fruit and vegetables. Doctors advise following a diet rich in fruits and vegetables (2–3 pieces a day) to reduce the risk of developing type 2 diabetes.

Medicines used to treat high blood pressure. High blood pressure, an excess of fat in the blood (cholesterol, triglycerides), obesity and diabetes collectively form the condition known as metabolic syndrome. It is important to manage each component independently.

A history of hyperglycaemia or diabetes during pregnancy. Individuals who have experienced elevated blood glucose levels associated with taking certain medicines or, in the case of women, during pregnancy are more likely to develop type 2 diabetes.

A family history of diabetes. People with first-degree (parents, siblings, children or grandparents) and also second-degree (aunts/uncles, nephews/nieces) relatives who have a history of diabetes present a greater risk of developing it themselves.
| Score | Risk of developing type 2 diabetes |
|---|---|
| Less than 7 | Low risk: An estimated 1 in every 100 people will develop type 2 diabetes |
| 7 - 11 | Slightly elevated risk: An estimated 1 in 25 people will develop type 2 diabetes |
| 12 - 14 | Moderate risk: An estimated 1 in 6 people will develop type 2 diabetes |
| 15 - 20 | High risk: An estimated 1 in 3 people will develop type 2 diabetes |
| Over 20 | Very high risk: An estimated 1 in 2 people will develop type 2 diabetes |
¿Qué puedo hacer?
- Si se tienen familiares con diabetes, procurar mantener un peso correcto. Un aumento del perímetro de cintura supone un riesgo mayor de tener diabetes tipo 2, mientras que si se practica ejercicio físico regular, disminuye este riesgo.
- Si la puntuación en el test de FINDRISK está entre 12-14, es conveniente disminuir el riesgo y hay que plantearse seriamente la práctica de ejercicio físico regular junto con unos buenos hábitos de alimentación. Consultar con su equipo de salud para futuros controles.
- Si la puntuación en el test de FINDRISK es superior a 15 puntos o más, consultar con su equipo de salud para descartar tener una diabetes aunque no tenga ningún síntoma.
- Se deben mantener las medidas preventivas de alimentación saludable y actividad física regular, que por otro lado son recomendables también para todas los miembros de la familia para promover un mejor estado de salud.
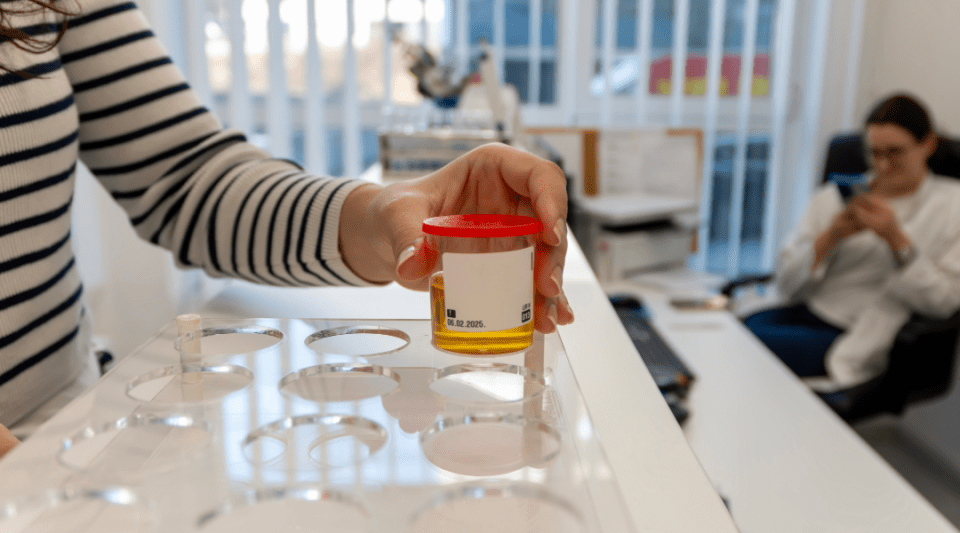
Diabetes is diagnosed by means of a blood test that determines a person’s blood sugar (glucose) levels. Normal blood glucose values range between 70 and 100mg/dL.
This test analyses whether the analytical indicators are:
- After fasting: equal to or higher than 126 mg/dL, in two measurements.
- At any time of the day: equal to or greater than 200 mg/dL accompanied by characteristic symptoms, such as an increased need to urinate or excessive thirst.
- After taking a glucose solution (75 g): above 200 mg/dL. This test is carried out on individuals whose glucose levels after fasting are between 100 and 126 mg/dL.
- Glycated hemoglobin (HbA1c): equal to or higher than 6.5%.
Treatment may vary depending on the stage in which the disease was first diagnosed and how it is evolving. Therefore, people with type 2 diabetes will follow different treatment plans:
- A healthy diet that helps control body weight in combination with regular physical exercise (at least 150 minutes/week) and oral medicines (metformin).
- If the first treatment is not enough, then the patient’s plan will incorporate new oral or injectable medicines.
- If the second treatment is insufficient, then insulin might have to be added to the treatment regime.
Oral drugs
Oral anti-diabetic drugs are tablets used to help regulate blood sugar levels. They are taken from the outset of treatment for type 2 diabetes. There are several types and different modes of action; it is, therefore, important that you are familiar with the effects and take them at the times indicated.
Your healthcare team will indicate when you should take them, whether before or after meals, and whether or not they involve the potential risk of producing sugar lows.

Sulphonylureas: stimulate an increase in insulin secretion from the pancreas.

Meglitinides: similarly, these also stimulate increased insulin secretion from the pancreas.

Biguanides: reduce the production of glucose in the liver.

Alpha-glucosidase inhibitors: delay and reduce the absorption of carbohydrates.

Thiazolidinediones: these decrease insulin resistance.

SGLT2 inhibitors: these reduce renal glucose reabsorption.

DPP-4 inhibitors: inhibit an enzyme that deactivates incretins, cause an increase in insulin secretion and inhibit glucagon secretion.
The drug of choice in all patients with type 2 diabetes is metformin (a biguanide), unless there is a specific contraindication or the individual presents clear symptoms that their body requires insulin. The metformin’s mechanism of action inhibits natural glucose production in the liver.
Injectable drugs

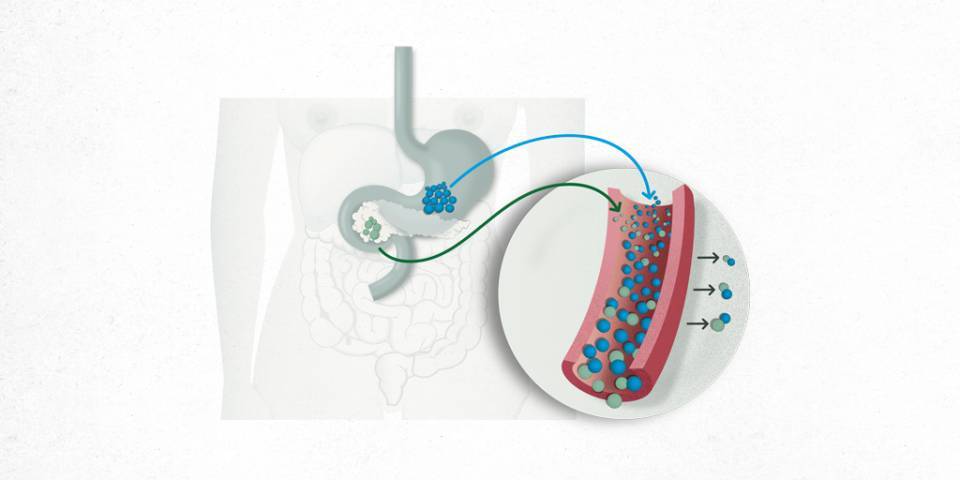
GLP-1 analogues. These medicines are administered subcutaneously. They increase insulin secretion, inhibit glucagon secretion and delay gastric emptying.
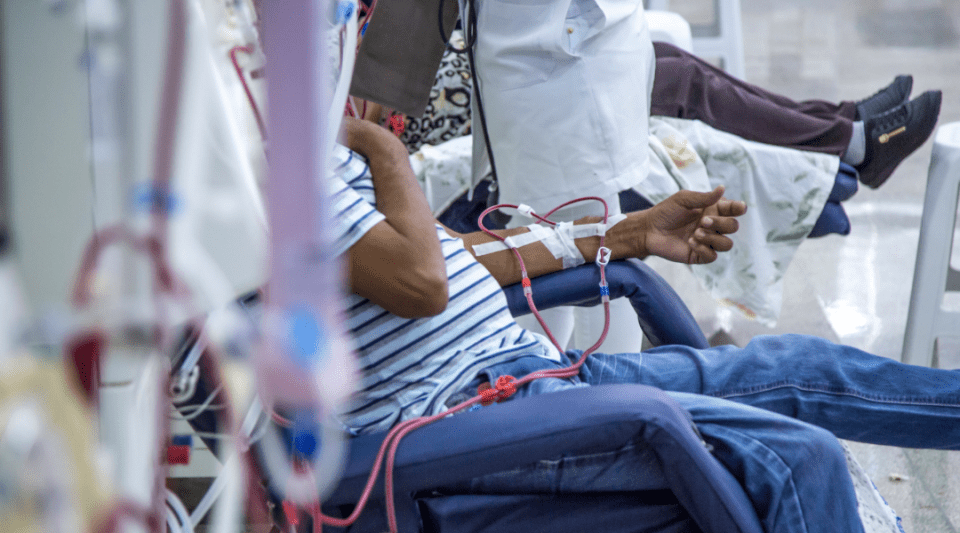
As the years pass, the large majority of people with type 2 diabetes eventually require insulin.
In general, everybody, with or without diabetes, should follow a healthy, balanced and varied eating plan. Eating plans should be customised according to the patient’s age, level of activity, timetable, body weight and personal preferences.
Advice for people with high blood pressure
To prevent and manage high blood pressure, patients must avoid being overweight and complete regular physical exercise. Recommended blood pressure values for people with diabetes are less than or equal to 130/80. In some cases, patients may require treatment and have to follow a salt-free eating plan.
| Recomended foods | Unrecomended foods |
|---|---|
| Use aromatic herbs and spices to season meals (garlic, parsley, bay leaves, mint, oregano, rosemary, thyme, etc.) | Salt, salted foods and any salted sauces (mustard, ketchup, pickles) |
| Salt-free bread and bakery products | Salted bread and bakery products |
| Salt-free soft cheeses | Hard cheeses |
| Mineral water | Sparkling water |
|
Use cooking methods that do not reduce the food’s natural flavour (grilling, steaming, baking, microwaving, baking in foil and frying in olive oil if you are not overweight) |
Confectionery and bakery products and any ready-made, pre-cooked or canned/preserved products. |
In cases of severe hypertension, or advanced kidney disease, your healthcare team can provide other specific recommendations and even warn you about foods with a naturally high salt content.
Advice for people with high cholesterol levels

We should all follow a diet that is low in animal fat (butter, lard, cured meats, red meats, etc.).

A person with diabetes is advised to maintain their total cholesterol below a level of 200 mg/dL. Values of less than 100 mg/dL are recommended for LDL (bad) cholesterol and greater than 40 mg/dL for HDL (good) cholesterol.

A sedentary lifestyle and being overweight are factors that can lead to an increase in LDL (bad) cholesterol. You may need to take medicines in combination with the dietary recommendations to control your cholesterol levels.

To prevent cholesterol levels from increasing you should try to avoid being overweight, which is a general recommendation for everyone, with or without diabetes.
Physical activity adapted to the abilities of each person and practised regularly can provide a very positive contribution to achieving good control over diabetes, reducing cardiovascular risk factors (obesity, high cholesterol, etc.) and improving one’s sense of mental and physical well-being.
In the case of type 2 diabetes, exercise constitutes an important part of treatment, as do diet and medication (tablets or insulin), and patients must ensure they exercise at least 150 minutes per week.
The exercise should be planned beforehand to avoid an excessive decrease in blood sugar (hypoglycaemia), especially in patients treated with insulin or any other type of medicine that could result in hypoglycaemia.
Collaboration between people with diabetes and their families and healthcare teams is essential for optimizing the treatment and, at the same time, for integrating it into their day-to-day life in terms of regular eating habits, timetables and physical activity.
Therapeutic education in diabetes is a learning process that provides the knowledge and skills required by people with diabetes and their families so they may actively take part in everyday treatment decisions.
Substantiated information by:





Published: 20 February 2018
Updated: 24 November 2021
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox