- What is it?
- Diagnosis
- Treatment
- Type 1 diabetes
- Type 2 Diabetes
- Gestational Diabetes
- Disease evolution
- Living with the disease
- Research lines
- Frequently Asked Questions
- Diabetes at the Clínic
- Gestational Diabetes at the Clínic
- Research at the Clínic
- Teaching and Training at the Clínic
- Team and structure
What is Gestational Diabetes?
Gestational diabetes is a type of the disease that presents during second half of pregnancy (gestation) in women with no prior history of diabetes. Gestational diabetes can affect the health of both the mother and the foetus, which is why it is so important to detect and treat it early on.
This type of diabetes usually appears in the third trimester of pregnancy as a result of the hormonal changes which occur. All pregnant women therefore undergo O’Sullivan’s test to diagnose its presence.
Expectant mothers can control gestational diabetes by eating correctly, performing regular exercise and, if necessary, by taking medication (usually insulin). Strict control over blood sugar levels can help prevent a difficult birth and problems with the baby.
Blood sugar levels will return to normal values shortly after childbirth. However, mothers who have experienced gestational diabetes present a greater risk of developing type 2 diabetes in the future. That is why they should continue to follow the preventive measures recommended by their healthcare team. Only some women who have had gestational diabetes continue with diabetis after childbirth.
To understand how gestational diabetes occurs, one must understand how pregnancy affects the metabolism of glucose.
The body directs the food it consumes to produce glucose (glucose) that enters the bloodstream. In response, the pancreas (a large gland behind the stomach) produces insulin. Insulin is a hormone that helps glucose to pass from the bloodstream into the cells of the body, where it is used as energy.
During pregnancy, the placenta, which connects with the baby, produces high levels of various hormones that cause resistance to the action of the insulin itself. Almost all of these hormones prevent the action of insulin in cells and, therefore, cause an increase in blood glucose levels.
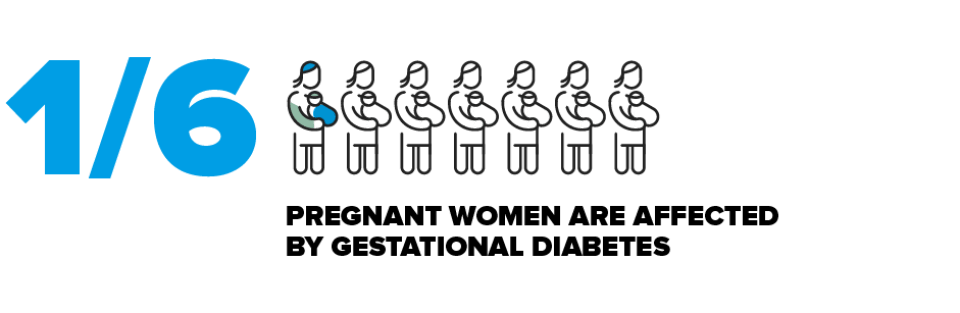
Gestational Diabetes is caused by the hormonal changes associated inherently with the actual pregnancy and can affect between 5% and 15% of pregnant women. The incidence varies according to area and diagnostic criteria. Globally, 1 in every 6 women will suffer from gestational diabetes. In Spain, approximately 9 out of 100 pregnancies cause the onset of gestational diabetes (9%).
Any woman can develop gestational diabetes; however, there are different risk factors associated with the condition such as:

A maternal age of over 35 years

Slightly elevated sugar levels without meeting the criteria for diabetes (prediabetes)

A history of gestational diabetes in a previous pregnancy

Having given birth to a baby weighing over 4 kg.

A family history of type 2 diabetes in parents or siblings

Being overweight or obese, with a body mass index (BMI) of 30 kg/m2 or more.

For unknown reasons, African, African-American, South American and Asian women are more likely to develop gestational diabetes.
Women with risk factors should, before becoming pregnant, make a determination of blood glucose (blood glucose) and those with overweight and obesity should go on a diet of slimming.
Patients do not usually notice any symptoms of gestational diabetes because the routine tests performed during pregnancy help identify the condition very early on. Nevertheless, if it is not detected early, then the patient could notice symptoms associated with increased sugar levels (hyperglycaemia) such as an excessive weight gain by gestational age, thirst and very urge to urinate.
Gestational diabetes, in general, does not present specific symptoms, but it can be suspected in some cases if there is an excessive weight gain, fatigue, thirst and urge to urinate. A blood test is necessary to make the screening.
This exam, known as O’Sullivan’s test, is carried out by administering 50 g of oral glucose at any time of the day and without the need for fasting or a special diet prior to the test.
If 60 minutes after taking the glucose, the individual’s blood glucose level is equal to or higher than 140 mg/dL (7.8 mmol/L), then the test result is considered positive and the patient will have to undergo an oral glucose tolerance test (OGTT) to confirm the diagnosis.
When is O’Sullivan’s test performed?

In the first trimester. In pregnant women with a high risk (over 35 years, obese, background of gestational diabetes, previous pregnancies that raised suspicions of gestational diabetes, a history of diabetes in first-degree relatives).

In the second trimester (weeks 24–28 of the pregnancy). All pregnant women with no previous diagnosis of diabetes (universal screening), including those with negative results from a screening test in the first trimester.

In the third trimester. Pregnant women who were not tested or whose O’Sullivan’s test result was normal in the second trimester, but who subsequently develop complications that suggest gestational diabetes, such as a foetus with an above average weight for its gestational age (macrosomia) and an excessive presence or increase of amniotic fluid around the foetus before it is born (polyhydramnios). This group of patients will directly undergo an OGTT.
Whenever O’Sullivan’s test is positive, the diagnosis is confirmed by means of an oral glucose tolerance test (OGTT).
Before carrying out this test, it is important to remember that either two fasting blood glucose levels of more than 126 mg/dL on separate days or a random test value greater than 200 mg/dL is sufficient to confirm the diagnosis of diabetes, thus eliminating the need for an OGTT.
To carry out the SOG, you must take into account:
- Fasting before 8-14 hours.
- Do not restrict your diet 3 days before. You must ensure a daily intake equal to or greater than 150 g of carbohydrates.
- During the test, you must be at rest and not smoking.
The day of the test is performed:
- A blood test.
- Subsequently, a drink containing 100 grams of glucose is ingested.
- Then, 3 more blood samples are obtained corresponding to 1h, 2h and 3h postingesta glucose.
The diagnosis of gestational diabetes is confirmed if two or more parameters in the blood test are greater than the following values:
- Basal value: 105 mg/dL (5.8 mmol/L)
- 1 hour: 190 mg/dL (10.6 mmol/L)
- 2 hours: 165 mg/dL (9.2 mmol/L)
- 3 hours: 145 mg/dL (8.1 mmol/L)
If only one parameter exceeds these limits, then the OGTT will be repeated in 4 weeks.
There are differences between the various diagnostic criteria. This section refers to the recommendations of the Spanish Diabetes, Obstetrics and Pediatric Societies, based on the National Diabetes Data Group, which are the most widely accepted.
Once you have been diagnosed with gestational diabetes then treatment should start as soon as possible. It is based around:

A healthy diet that helps control body weight and blood sugar levels. Patients should not exceed a maximum weight gain of 11-15 kg of weight gain (if the pregnant woman had a normal pre-pregnancy weight) or less if she was already overweight or obese. A healthy diet must include foods from all the groups: dairy, grains, fruit, vegetables, proteins and fats. Your customised food intake should be distributed over 5–6 small meals (breakfast, lunch and dinner, supplemented at mid-morning, mid-afternoon and before going to bed) so you do not go too long without eating anything and to prevent ketone production. The diet plan should be individualized according to the habits of the patients, the nutritional needs of the pregnancy and the blood sugar levels.

The diet plan should be based on approximately 2,000–2,500 kcal. Approximately 45–50% of these calories must be carbohydrates, with 20% proteins and 30% in fats.

You must eliminate foods and drinks rich in fast-absorbing carbohydrates from your diet (sugar, sugary drinks, sweets, chocolates, cakes). You can use aspartame as a sweetener.

To ensure you have optimal blood sugar levels 1 hour after each meal, it is very important you eat meals that are similar, in terms of carbohydrate-rich foods, proteins and fat, to those recommended for you.

Regular physical exercise. The recommendations are the same as for any other pregnant woman. Additionally, exercise can help regulate your blood sugar levels.

Check your blood sugar levels (capillary blood glucose test) before and 1 hour after each meal (pre- and postprandial).
Ask your healthcare team what you should do if your sugar levels exceed these target values:
|
Time of day |
Target values |
|---|---|
|
Fasting and before meals |
No more than 95 mg/dL (5.3 mmol/L) |
|
1 hour after a meal |
No more than 140 mg/dL (7.8 mmol/L) |
|
2 hours after a meal |
No more than 120 mg/dL (6.7 mmol/L) |

Monitor your ketones in urine levels. The presence of ketones during pregnancy is undesirable because it can affect the foetus’ psychomotor development. Ketones may be present in the urine if you go a long time without eating or if your diet is inadequate. In pregnant women who take insulin, the presence of ketones may also indicate they require more insulin.

Therapeutic education about daily treatment self-management. It is important for patients and their families to acquire the knowledge, techniques and correct attitudes required to achieve good treatment adherence, to improve the health of both mother and child, and to prevent complications associated with poorly controlled gestational diabetes.
If following this treatment does not achieve the desired sugar control goals, treatment with insulin will have to be added. This drug has been shown to reduce the occurrence of adverse events for both mother and foetus when added to the diet.
The adequate treatment of gestational diabetes that helps maintain the glycemic level similar to that of non-diabetic pregnant women, minimizes in an extraordinary way the risk that the fetus presents any of these complications. In this sense, it is essential that the diagnosis and, consequently, the treatment is as early as possible. The diagnostic strategy of gestational diabetes is based on the universal practice of screening.
The onset of uncontrolled gestational diabetes could have consequences for both the foetus and mother.
Risk of complications for the baby associated with gestational diabetes
- Excessive birth weight. The excess of glucose in the blood stream crosses the placenta and causes the foetus’ pancreas to generate more insulin. This can mean the baby grows too big (macrosomia). Very large babies (weighing over 4 kg) are move likely to experience problems when passing through the birth canal, suffer birth injuries or require a caesarean section delivery.
- Premature. Sometimes, if the baby is very large, the doctor may recommend a premature birth. Preterm births can increase the risk of breathing difficulties (respiratory distress syndrome) and the baby may require assisted breathing until their lungs mature. Regardless of the above, babies born to mothers with gestational diabetes can still suffer respiratory distress syndrome including when they are born full term, because their lungs will mature later than the babies of non-diabetic mothers.
- Low blood sugar levels (hypoglycaemia). Babies born to mothers with gestational diabetes sometimes have low blood sugar levels (hypoglycaemia) shortly after birth because they are producing high levels of insulin. Severe episodes of hypoglycaemia may produce convulsions in the baby. This complication is treated with the intravenous administration of a glucose solution to bring the baby’s blood sugar back up to normal levels.
- Type 2 diabetes in the future. Babies whose mothers had gestational diabetes present a greater risk of developing obesity and type 2 diabetes.
Risk of complications for the mother associated with gestational diabetes
- High blood pressure and pre-eclampsia. It is very important to control blood pressure during the pregnancy. Pre-eclampsia is a serious, life-threatening complication for both mother and child.
- Risk of gestational diabetes repeating in future pregnancies.
- Increase the risk of developing type 2 diabetes in the future.
There are differences between the various diagnostic criteria in use. This section refers to recommendations made by the Spanish Societies for Diabetes, Obstetricians and Paediatricians, which are based on the National Diabetes Data Group and are the most widely accepted.
It is worth remembering that once the baby has been born this type of diabetes “cures itself” in the vast majority of women. It is a good idea to repeat the glucose curve between 6-8 weeks after the birth it is convenient to repeat oral glucose overload (SOG) with 75 g of glucoseto confirm the condition has resolved itself.
Women who plan a further pregnancy face the risk of suffering from gestational diabetes once again. Statistics show that 30 in 100 women (30%) may develop another case of gestational diabetes if they get pregnant again. It is very important that you tell the gynaecologist that you have had gestational diabetes when planning a new pregnancy.
There is also the risk of developing type 2 diabetes “that doesn’t cure itself” over the course of time, especially during the first 5 years after the birth. There is a lot of variation in the number of women reported to develop postnatal type 2 diabetes. For example, some studies show that at 3.5–6.5 years postpartum 62 out of 100 women (62%) suffered from type 2 diabetes, while in Spain, just 11 in 100 women (11.5%) developed type 2 diabetes in an 11-year period after the birth.
Children of mothers who had gestational diabetes also have a greater risk of developing type 2 diabetes. The good news is that type 2 diabetes can be prevented by following a healthy diet and taking part in regular exercise (at least 150 minutes per week). Incorporating these habits into your lifestyle not only helps prevent type 2 diabetes, but they also improve your overall state of health. Eating a healthy diet and carrying out regular exercise are excellent habits for a healthy lifestyle for the whole family.
Substantiated information by:





Published: 20 February 2018
Updated: 24 November 2021
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox