- What is it?
- Diagnosis
- Treatment
- Type 1 diabetes
- Type 2 Diabetes
- Gestational Diabetes
- Disease evolution
- Living with the disease
- Research lines
- Frequently Asked Questions
-
The disease at the Clínic
- Team and structure
Diabetes treatment
Diabetes is a chronic disease and does not have a cure, except for the case of gestational diabetes which usually disappears after childbirth. Treatments have improved a great deal in recent years and research continues to discover preventive strategies and new treatments.
Blood glucose monitoring, insulin and oral medicines may all form part of your diabetes treatment depending on the type you have. It is also important to follow a healthy eating plan, maintain a healthy weight and perform regular physical exercise.
It is essential to highlight the differences between the types of diabetes and their treatments.
Type 1 diabetes
People with type 1 diabetes mellitus have to:
- Inject insulin in order to stay alive.
- Monitor their blood glucose levels.
- Follow a balanced eating plan.
- Complete regular physical activity.
Type 2 diabetes
Treatment may vary depending on the stage in which the disease was first diagnosed and how it is evolving. People with type 2 diabetes mellitus will therefore follow different treatment plans:
- Follow a healthy eating plan to help control body weight, carry out regular physical exercise (over 150 minutes per week) and take oral medicines
- If the first treatment is not enough, then the patient’s plan will incorporate new oral or injectable medicines
- If the second treatment is insufficient, then insulin might have to be added to the treatment plan. The frequency of blood glucose analyses will depend on the type of treatment
Gestational diabetes
Treatment is based on:
- Following a healthy eating plan
- Completing regular physical activity
- Measuring blood glucose just before and one hour after each meal
If this treatment plan does not meet the desired objectives in terms of managing glucose levels, then insulin will be added to the regime since oral antidiabetic medicines cannot be taken during pregnancy.
Treatment self-management
Patients have a very important role when it comes to managing the disease and it is calculated that they make 90% of decisions regarding their own treatment. Therefore, an understanding of the disease and how to manage their treatment are vitally important for both people with diabetes and their family members or carers.
This treatment self-management requires patients:

Follow a healthy diet

Realise regular physical exercise

Monitor their blood sugar levels

Take their medication (insulin [injections] or tablets)

Know how to cope with hypoglycaemia/hyperglycaemia

Reduce the risks (acute and chronic complications)

Acquire healthy lifestyle habits

In the case of type 1 diabetis, the drug treatment is always insulin from the diagnosis of the disease.

In the case of type 2 diabetes, the drug treatment will vary according to the disease's diagnosis and evolution.

In the case of gestational diabetes, the drug treatment, if it is necessary, will always be insulin for the contraindication of the oral drugs.
In general, everybody, with or without diabetes, should follow a healthy, well-balanced and varied eating plan in order to:

Maintain a correct nutritional status and weight.

Help manage their blood sugar levels.

Prevent and/or treat cardiovascular risk factors such as high blood pressure and high cholesterol levels (hypercholesterolemia).
All eating plans should be customised according to the patient’s age, level of activity, timetable, body weight and personal preferences.
-
Maintaining a correct nutritional status and weight
A healthy eating plan must include foods from all the groups: dairy, fruits, vegetables and/or salads, grains, proteins and fats. The quantities of milk products (dairy), fruits and vegetables are recommendable for everyone, regardless of age and body weight. The quantities of grains, proteins and fats must be adjusted to each patient’s body weight and level of physical activity.

Dairy: 2–3 times a day, preferably skimmed or semi-skimmed.

Fruit: 2–3 pieces per day. Vegetables:

Vegetables are recommended for everyone, regardless of age and body weight.

Grains: Grains include bread, biscuits, pasta, but also things like potatoes, pulses, peas, semolina, etc. Daily quantities are determined according to the patient’s body weight and normal level of activity.

Fats: Fatty foods contain the most calories, independent of whether it is animal or vegetable fat. However, the difference between them lies in the fact that animal fat (butter, single and double cream, and fat in meat, cured meats, cheese, etc.) has much higher levels of cholesterol and saturated fat.
Vegetable fats: olive oil and nuts. Vegetable fat is healthier, with the exception of coconut and palm oils. It is a good idea to use olive oil for cooking and adressing. Margarine is a vegetable-based fat but its properties are like those of a saturated fat. Recommendations are to eat 30 g of nuts per day.
Animal fats: single cream, double cream, butter, mayonnaise, lard and fats in industrial confectionery and bakery products. It is important to avoid eating them regularly because they have a high cholesterol and saturated fat content.
One soup spoon of oil contains around 100 calories, as does an individual portion of butter. Overweight people have to control the type and amount of fats they consume in their diets and avoid cooking techniques that use a lot of oil, e.g., shallow and deep frying. People with a correct weight still have to control the type of fat but not the daily amount.

Protein foods: meat, fish, poultry, cheese and cured meats. Recommendations for meat portions are 100 g and, if possible, choose leaner meats (skinless chicken, rabbit, etc.) because they contain less cholesterol and saturated fat. You should increase how much fish you eat, both white and blue fish, with recommended serving sizes of 150 g.
A variety of eating patterns are acceptable for the treatment of diabetes. In our environment, one of the dietary patterns that has proven beneficial for health (helps prevent type 2 diabetes and reduce the incidence of cardiovascular events) is the Mediterranean diet pattern.

Drinks. Water, soda, tea, coffee and light drinks can be freely consumed.

Refreshments. Consumption of soft drinks containing sugar, fruit juices or nectars, shakes, etc. is discouraged. Remember that a can of soda with sugar brings the equivalent of four sachets of sugar.
People with diabetes have to control their intake of carbohydrate-rich foods (also known as carbs or sugars) in each meal, since this type of foods have a direct effect on blood sugar levels.
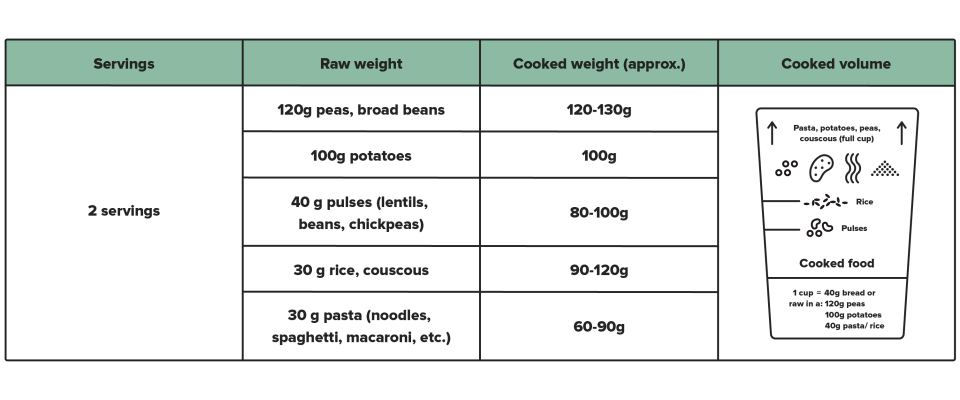
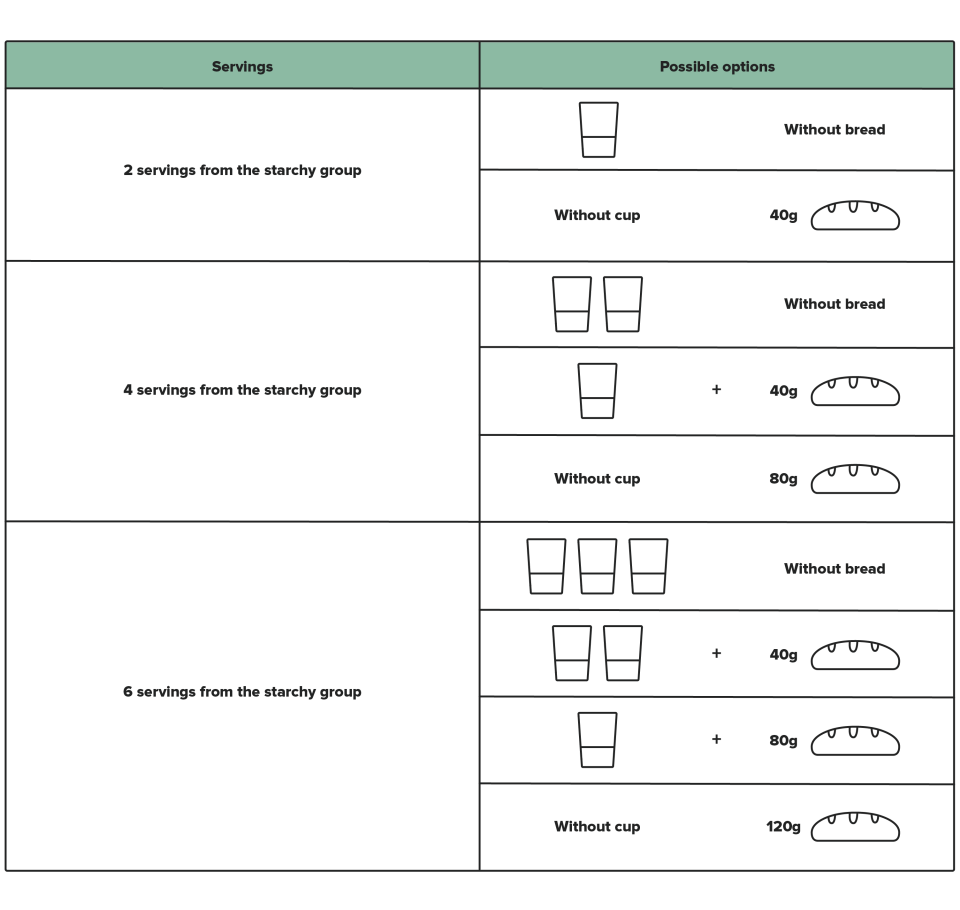
The measuring cup is an instrument which lets you measure and swap foods in the STARCHY group: potatoes, pasta, peas, broad beans, couscous, pulses (lentils, chickpeas, and haricot beans), rice, and bread.
1 measuring cup filled to the mark shown for each food, after cooking, is the equivalent of 40 grams of bread.
The main advantage of measuring and swapping these cooked foods, and being able to swap them for 40 gram pieces of bread, is that this gives you an easy way to:
- Vary menus with the same values
- Adapt the recommended meal plan to available meals at home or work
How to use the measuring cup?
According to the number of servings from the STARCHY group recommended in your diet plan, you can swap foods as in the following examples.
It is very important that your attending healthcare professional designs an eating plan adapted to your individual needs, dietary habits, timetables and level of activity. It is also imperative that patients have the knowledge and skills required to vary their menus but while maintaining equivalence. Diabetes a la carta website is a resource where you can find equivalences and menus adapted to the ration system.
Physical activity adapted to the abilities of each person and practised regularly can provide a very positive contribution to achieving good control over diabetes, reducing cardiovascular risk factors (obesity, high cholesterol, etc.) and improving one’s sense of mental and physical well-being.
Exercise serves different functions depending on the type of diabetes.
- In the case of type 1 diabetes, exercise is recommendable simply to maintain a good physical condition.
- In the case of type 2 diabetes, physical activity constitutes an important part of treatment, as do diet and medication (tablets or insulin), and patients must ensure they exercise at least 150 minutes per week.
The exercise must be planned beforehand to avoid an excessive decrease in blood sugar (hypoglycaemia), especially in patients treated with insulin or any other type of medicine that could result in hypoglycaemia. In any case, you should consult your healthcare team about:
- The type of exercise
- Duration
- Frequency
- Intensity
All of these factors are important before starting any type of physical activity, as are recommendations regarding making adjustments to your treatment before, during and after exercising, if necessary.
You can find different aspects related to exercising, as well as videos with different types of exercises, at web Diabetes a la carta.
What is a capillary blood glucose test?
It is a technique used to measure your blood sugar levels. A single drop of capillary blood is introduced into a meter that subsequently gives a reading of your glucose level. This measurement tells us if the blood glucose level is correct, too high or too low.
What do I need?

A measuring device, called a glucometer.

Blood lancets for finger pricking. Preferably with an automatic needle.

Test strips compatible with the meter.

Cotton wool or paper tissues.

A management notebook or mobile application for recording results.
The values recommended by the American Diabetes Association are:
- Fasting and before meals: 80–130 mg/dL
- 2 h after a meal (postprandial): less than 180 mg/dL
These values have to be customised to each case and their flexibility depends on the patient’s objectives: the duration of diabetes, age, the presence of other diseases, macro- (cardiovascular disease) and microvascular complications, undetected hypoglycaemia or other individual considerations. You should talk with your healthcare team to find out what your objectives are.
How often do I have to do a capillary blood glucose test?
The number of capillary blood glucose tests depends on the type of treatment required for your diabetes.
- In the case of type 1 diabetes, from the outset, you will have to perform the test at least 3 or 4 times a day and learn how to interpret the results so you can adjust the insulin according to your sugar levels and intake of carbohydrate-rich foods.
- If you have type 2 diabetes, then you will be advised to perform a specific number of capillary blood glucose tests in function of your treatment. Some patients with type 2 diabetes may not have to measure their capillary blood glucose level.
| Type of treatment | Stable blood glucose control | Unstable blood glucose control |
|---|---|---|
| Non-pharmacological measures | 0 | 1/day or 1 weekly profile |
| Medicines that do not cause drug-induced hypoglycaemia | 0 | 1/day or 1 weekly profile |
| Medicines that cause drug-induced hypoglycaemia | 1/week | 1/day or 1 weekly profile |
| Basal insulin | 3/week | 2-3/day |
| Biphasic or intermediate insulin in 2–3 doses | 1-3/day | 2-3/day + 1 weekly profile |
| Basal-bolus insulin therapy | 3-4/day + 1 weekly profile | 4-7/day |
| Insulin infusion pumps | 4-10/day | To be customised |
-
How do you perform a capillary blood glucose test?

Wash your hands with soap and water. Rinse them well. You do not need to use alcohol, unless you cannot wash your hands. If this is the case, wipe your finger five times with alcohol-soaked cotton wool, particularly if you have touched fruits or sweet foods.

Prick the side of your finger. Avoid the tips of your fingers as this area is more sensitive to pain.

Follow the advice of your healthcare professional regarding the proper use of the glucometer and make sure you apply the drop of blood to the test strip correctly.

Record the result in your diabetes management notebook. Management notebooks provide a useful record of your blood sugar levels, as well as what medication you have taken or injected, and any incidents. They also represent a means of communication with your healthcare team.

Apart from management notebooks, mobile devices currently feature a range of applications that function as a notebook and can also store and perform different types of results analysis. There are also applications available for counting the portions of carbohydrates consumed.
Other methods of measuring blood sugar levels using interstitial glucose sensors are available. Continuous glucose sensors produce a “film” of the real-time evolution of blood sugar levels and so the patient can use this information to act accordingly and prevent increases or decreases in their glucose level. Glucose monitoring systems prove particularly useful in patients prone to suffering low sugar levels (hypoglycaemia), particularly in cases where they go undetected or occur predominantly at night.
A disadvantage of continuous glucose monitoring systems is that measurements are made in subcutaneous tissue, where the glucose concentration reaches the same level as the one measured in blood but after a certain delay (i.e., a value measured by one of these systems corresponds to the blood glucose level 15 minutes before the subcutaneous measurement).
Nowadays these systems can be connected to insulin infusion pumps with compatible features and, through the use of some algorithms, automatically stop and restart insulin administration. Patient participation is still vital in all of these systems. At present, they do not act as an artificial pancreas. These systems are not covered by the national health system in Spain and they must be self-financed by patients with diabetes.
Collaboration between people with diabetes and their families and healthcare teams is essential for optimizing the treatment and, at the same time, for integrating it into their day-to-day life in terms of regular eating habits, timetables and physical activity.
Therapeutic education in diabetes is a learning process that provides the knowledge and skills required by people with diabetes and their families so they may actively take part in everyday treatment decisions and can:

Understand diabetes and its treatment principles.

Learn the techniques used in capillary blood glucose tests and for injecting insulin

Prevent and know how to cope with acute complications (hyperglycaemia and hypoglycaemia).

Adapt their meal plan to their daily timetable and normal level of activity.

Prevent vascular risk factors: smoking, cholesterol, high blood pressure, etc.

Prevent foot lesions, in at-risk patients.

Attend regular check-ups.

Understand that correct management of their diabetes improves their quality of life.
“Diabetes self-management education” is defined as a patient-centred approach designed to meet their needs and provide resources, values, and strategies, equipping patients with improved understanding, skills, and attitudes concerning their condition and its treatment. Ultimately, this results in better quality of life, greater therapeutic adherence, and fewer complications.
One of the theories that lend its name to this process is that of “Empowerment”, which is defined as “a state of mind in which individuals or groups gain control over certain aspects of their lives by means of a more proactive and participatory role”. These points need to be addressed in the descriptions of problems on the Clinical Portal.
Information and therapeutic education help promote patient empowerment, so patients are free to make their own informed decisions. Both education on an individual basis and in a group with other patients and family members favour empowerment.
There are seven dimensions favouring patient empowerment associated with the management and treatment of the disease that should be taken into account:
| Dimension | Empowerment in each of the following dimensions means the person with diabetes: |
|---|---|
| Physical |
|
| Functional |
|
| Cognitive |
|
| Social |
|
| Experience |
|
|
Economic |
|
| Ethics |
|
Substantiated information by:





Published: 20 February 2018
Updated: 24 November 2021
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox