- What is it?
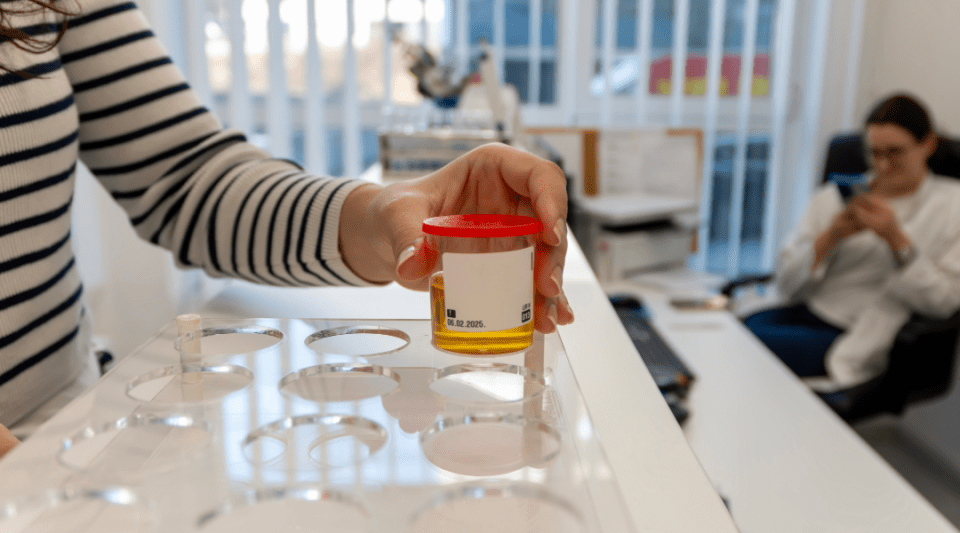
- Diagnosis
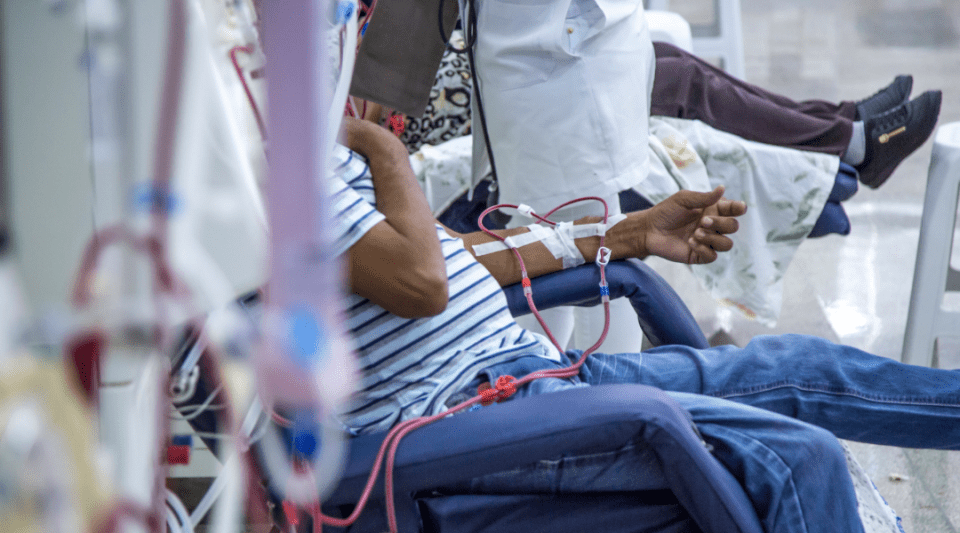
- Treatment
- Type 1 diabetes
- Type 2 Diabetes
- Gestational Diabetes
- Disease evolution
- Living with the disease
- Research lines
- Frequently Asked Questions
- Diabetes at the Clínic
- Gestational Diabetes at the Clínic
- Research at the Clínic
- Teaching and Training at the Clínic
- Team and structure
Living with Diabetis
Diabetes is a chronic disease that patients must learn to live throughout their entire lives. On an emotional level, this can mean patients go through different cyclic stages and may need support.
The diagnosis of a chronic disease implies an end to the patient’s previous health status. To adjust to their new medical condition, patients need to initiate a series of adaptive psychological mechanisms which entails passing through different stages: initial denial or shock, protest, anxiety, active negotiation and adaptation, “It would be better if I did not have diabetes, but I have to learn to live with it.” This adaptive process varies greatly between each person with diabetes and also between family members; those involved may experience it separately and at different times.
Regardless of these differences, patients with diabetes, given that they have a chronic illness, may undergo different psychological, family, social and also financial changes.
Therapeutic education programmes that integrate individual and group sessions (with other people with diabetes and their families) also provide an initial aid in this adaptive process. Even with this support, some people are unable to adapt psychologically and require specific professional help from a psychologist or psychiatrist. Currently, the figure of the psychologist is not integrated in most of the interdisciplinary teams that care for people with diabetes in our environment.
The latest guidelines published by the American Diabetes Association (ADA) stress that emotional well-being is an important part of diabetes care and self-management for patients and/or their families. Psychological and social problems can compromise the patient’s and/or family’s ability to complete daily diabetes treatment self-management tasks.
The ADA has prepared a series of standards regarding emotional aspects:
- Psychosocial support must be patient-oriented in order to benefit everybody with diabetes; it must count on their collaboration and should aim to optimise health outcomes and patient quality of life.
- Psychosocial screening, which may include: attitudes about the illness, expectations for treatment self-management and outcomes, mood, diabetes-related quality of life, available resources (financial, social and emotional), and psychiatric history.
- Providers should consider assessment for symptoms such as distress, depression, anxiety, eating disorders and cognitive disorders using standardised and validated tools at periodic intervals. Including caregivers and family members in this assessment is recommended.
- Consider screening older adults (aged ≥ 65 years) with diabetes for cognitive impairment and depression.
Associations for people with diabetes can also offer patients another type of support, by giving them the opportunity to meet other people in the same situation, by providing support in schools, offering legal advice, giving informative talks, demanding quality care, stimulating research into diabetes, etc. Ask for information about these associations in your reference centre.
A patient with diabetes can travel without any problems; they just need to plan their journey.

Take your medication and devices for controlling your diabetes.

Take foods that can provide you with the necessary carbohydrates in the event of hypoglycaemia.

Medical record with your treatment and evolution of the diabetes.

You can try new foods, but you must still control your diet, especially your carbohydrate intake.

Vaccinations. Vaccines are used to prevent infectious diseases, which are a common cause of high blood sugar levels (hyperglycaemia). Vaccines are not contraindicated in patients with diabetes. Patients should learn about vaccination requirements according to the country or countries of destination.

Preferably choose footwear made of soft, flexible leather, it should be lined, have no internal stitching and adapt to the anatomical shape of your feet.

It is advisable to take everything you need to carry with you from your own country, doubling or tripling the amount needed and sharing it among your travel companions.
All destinations are possible when planning a journey, so long as you take into account a series of recommendations. Generally speaking there is no reason why you should limit the frequency or type of journey. However, if you go through a period of unstable diabetes control or have an intercurrent illness, then you should consider delaying the trip. When packing your suitcase, do not forget:
Medicines and equipment used to control your diabetes
- Sufficient insulin and/or oral antidiabetics. It is better to double or triple the amount required. Always carry them in your hand luggage. If travelling with others, share the medication to avoid losing it all at the same time.
- Insulin syringes or pens.
- Glucometer and test strips.
- Test strips for ketones in urine, if you have been advised to use the test.
- Glucagon, if the medication you take has the potential to cause sugar lows (hypoglycaemia).
Food
- Foods to correct episodes of hypoglycaemia: sugar, glucose tablets or gels, fruit juice, etc.
- Non-perishable foods that you can use to improvise a meal that ensures an adequate supply of carbohydrates: Melba toast, juices in cartons, biscuits, etc.
Documentation
- Medical report including the most relevant points of your treatment and clinical progression. It should be written in English, if possible, so that it is more readily understood if you travel to foreign countries.
- Identification card, medical alert jewellery, etc. (optional).
Treatment regimen
- You must follow your usual treatment regimen, although you can incorporate some changes. You will need to perform capillary blood glucose tests more often as many factors can affect your blood sugar levels when travelling, e.g., the excitement of visiting a new country, a change of time zones, increased physical activity and different food.
- If you are on a subcutaneous insulin infuser, it is important to carry the alternative insulin regimen and insulin pens (rapid and slow) with you in case it breaks down during the trip.
Diet is an essential part of diabetes treatment. Having diabetes does not have to stop you from enjoying good cuisine. Travelling also implies trying out new foods and new cooking methods. There is no need to deprive yourself of this pleasure while also maintaining control over your diabetes.

The foods you must control the most are those rich in carbohydrates; note the amounts you eat at home before going travelling so you have a good mental image and can subsequently eat similar quantities. Use bread or fruit as back-ups if the meal has fewer carbohydrates than you usually eat or to improvise a meal under any conditions and anywhere.

If you eat a sweet dessert as well, then you obviously need to eliminate some carbohydrates from the total eaten in the meal. For example, if you try a slice of cake, you have to remove fruit and bread from that meal.

During the trip, it is crucial that you eat approximately your normal total intake of carbohydrates with each meal, even if you vary the type of food. Capillary blood glucose measurements will help you assess the results of these dietary changes.
Traveller’s diarrhoea is the most common health problem experienced by people who travel to developing countries.
- Increasing the frequency of capillary blood glucose tests will help you modify your insulin regimen, if necessary. The infection causing the diarrhoea can induce hyperglycaemia (high blood sugar levels) but a reduction in food intake and the diarrhoea itself can lead to hypoglycaemia (low blood sugar levels).
- Try to ensure, insofar as possible, your eating plan includes carbohydrate-rich foods and preferably choose the most astringent boiled starchy foods (rice, semolina, etc.) and apple (boiled or uncooked and grated).
- If you have vomited and your ketones in urine test is positive, go to your nearest hospital immediately.
The best option is to take everything you need to carry with you from home, doubling or tripling the amount, if necessary, and sharing it among your travel companions as a safety measure.
Insulin concentration
- Types of insulin administered via cartridges (pens) have a concentration of 1/100 everywhere around the world, but insulin in vials may not have the same concentration. In some countries insulin in vials is still marketed in concentrations of 1/40. Obviously a syringe with a 1/40 concentration cannot be used to extract 1/100 insulins and vice versa, another reason why you should always carry 2–3 times more insulin than you require and, even better, share it between several travel companions and always carry in hand luggage.
- X-ray scanners used at airport security controls will not alter the effects of your insulin.
Insulin storage conditions
- Avoid exposing insulin to light and extreme temperatures, anything below 0 °C or above 30 °C. These factors could affect the effectiveness of the insulin. In some cases, you may need to use a cool-box or isothermal bag.
- Once damaged by heat, rapid-acting insulin can take on a yellowish colour. NPH or slow-acting insulins may not mix correctly and the absorption retarding particles may stick to the glass vial.
Regulations for carrying insulin on airplanes
- Medicinal products, including liquids such as insulin, are exempt from carry-on rules for liquids and can be carried in hand luggage for subsequent use during the flight.
- Medicinal products must be individually identified at airport security controls, but they do not have to be carried inside a plastic bag.
- Recommendations are to carry the corresponding prescription or medical report with the medicinal products.
- It is also a good idea to get in touch with the airline because each has their own procedures regarding carrying these items inside airplanes. You can obtain more information at the company’s website.

The low temperatures in the airplane’s hold, where checked luggage is transported, can damage insulin and/or capillary blood glucose meters.

Travelling by boat can be very pleasant if you do not get seasick. If you do, it is better to avoid this means of transport or take motion sickness medicine before the journey or as soon as the first symptoms appear.
• If you take oral antidiabetics or insulin to treat your diabetes and seasickness causes you to vomit, it could lead to hypoglycaemia. Inform your travel companion or the boat’s crew about your diabetes so they may administer glucagon if required.
• If you vomit, measure your capillary blood glucose and decide whether you can wait the 15–30 minutes required to eat or drink and be sure of digesting some carbohydrate-rich foods: tea with sugar, fruit juice, Melba toast, etc. • However, if your capillary blood sugar level is less than 80 mg/dL, drink sugared water immediately in small sips and ensure somebody is present who can inject you with glucagon if necessary (loss of consciousness).

Train journeys can be very long. Respect your medication and meal schedules to avoid losing control over your diabetes. Ensure you know the restaurant car’s opening and closing times.

Organised tours may not fit in with your meal schedule. Always remember to carry foods in your hand luggage for improvising a meal: Melba toast, biscuits, fruits, etc.
- If you drive, stop to rest every two hours.
- Always measure your capillary glucose level before driving to minimise the risk of suffering an episode of hypoglycaemia while at the wheel, particularly if you have not eaten for hours and it is a long journey.
- If your sugar level is between 75–90 mg/dL, eat some extra food or drink a carbohydrate-rich drink, for example: 1 piece of fruit or 1 fruit juice or 1 glass of a sugary drink.
- If the reading is between 50–75 mg/dL, eat/drink the same amount plus 2 rusks or biscuits and do not start driving until you have confirmed your capillary sugar level is at least 100 mg/dL.
- If the test measures less than 50 mg/dL or you have symptoms of hypoglycaemia (cold sweat, tremors, dizziness, palpitations, disorientation, lack of concentration, etc.), treat the hypoglycaemia with sugar, fruit juice or sweets, etc. and do not start driving until you have confirmed your capillary sugar level is at least 100 mg/dL. Remember that you do not fully recover the ability to react until a few hours after an episode of hypoglycaemia.
- Always carry sugary foods or drinks with you (sugar, fruit juice, sweets, etc.) so you can treat hypoglycaemia wherever you may be.
- Also store biscuits, Melba toast, bread or other similar foods in the car as a substitute for a meal in case of a traffic jam, etc.
- Excessive alcohol reduces reflexes when driving and can also mean the symptoms of hypoglycaemia go unnoticed.
- You should not drive if you have drunk alcohol and maximise precautions if you normally find it hard to recognise the symptoms of hypoglycaemia.
- It can get very hot inside an unattended parked vehicle, especially in summer; the high temperatures reached can damage insulin. Never leave your insulin in a car. Always carry it with you.
- Similarly, if in cold areas during winter, the temperature can fall below 0 °C and insulin can be damaged by freezing. Carry it with you at all times.
If you inject insulin, then besides following the general recommendations, and depending on the characteristics of the trip, you may previously need to discuss adapting your regimen with your healthcare team. Any changes made will relate to:
- Your treatment regimen
- The journey departure time and duration
- The time difference based on the longitude of the destination country
In general, if you are following a multi-dose insulin regimen (rapid-acting insulin before meals and long-acting insulin once or twice a day), then it is better if you just inject rapid-acting insulin every 4–5 hours during the journey as its short-lived action makes it easier to manage and also provides greater flexibility in your diet.
When you reach the destination country, adjust the long-acting insulin according to your normal schedule.
- If you travel west, the day is longer. For example, when it is 8 pm in Spain, it is 2 pm in New York. You will therefore need an extra dose of rapid-acting insulin in order to adjust your regimen to the destination country’s time zone.
- If you travel east, the day is shorter. For instance, when it is 8 pm in Spain, it is 2 am in Bangkok. And so you will need to eliminate a dose of rapid-acting insulin in order to adjust to the destination country’s time zone.
- Patients who use continuous subcutaneous insulin infusion systems will need to set the time on the pump to local time when they reach the destination country, and then reverse this adjustment when they return home.
- Ensure you take more than one pair of suitable footwear with you and which you have already worn at home for a while. We tend to walk more than usual when travelling, both in the country and in the city.
- Never walk bare foot if you present a high risk of suffering foot injuries due to a loss of sensitivity to pain (neuropathy) or vascular problems (vasculopathy). In such cases maximise your foot care.
- Follow foot hygiene recommendations.
- Check your footwear every day before putting it on. Feel around inside with your hands to ensure there are no foreign objects (loose seams, stones, pins, etc.)
- Remember your footwear should preferably be made of soft, flexible leather, it should be lined, have no internal stitching and adapt to the anatomical shape of your feet. They must have a wide heel, 1–4 cm. Try to avoid shoes that are completely flat, open-toed or lack any support.
Substantiated information by:





Published: 20 February 2018
Updated: 24 November 2021
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox