Frequently asked questions about Tuberculosis
It is true that, in Spain, as in other Western countries, the incidence of tuberculosis has decreased substantially in recent decades, but it has never gone away completely.
In Catalonia, about 12 new cases per 100,000 inhabitants per year are diagnosed, with some disadvantaged areas of Barcelona having an incidence 10 times higher. The tuberculosis germ is acquired through contact with a person who is sick with pulmonary tuberculosis.
The source of infection is often not known; among other reasons, because it may have occurred months or even years before the symptoms of the disease appear. In fact, most people who come into contact with the tuberculosis germ (up to 90%) will never develop the disease, because the immune system will be able to kill the germ or at least contain it harmlessly long term, throughout the person's life.
It is true that people with immune problems or those receiving immunosuppressive treatment are more predisposed to contracting tuberculosis.
Some relatively common conditions, such as diabetes mellitus, kidney failure or certain toxic habits, such as alcohol abuse and smoking, are also predisposing factors.
Most patients do not have any significant immune disorders but, during admission or in the outpatient clinic, the physician will perform routine tests to rule out serious immune problems or other diseases that predispose to infection. It is mandatory, for example, to request tests for HIV infection.
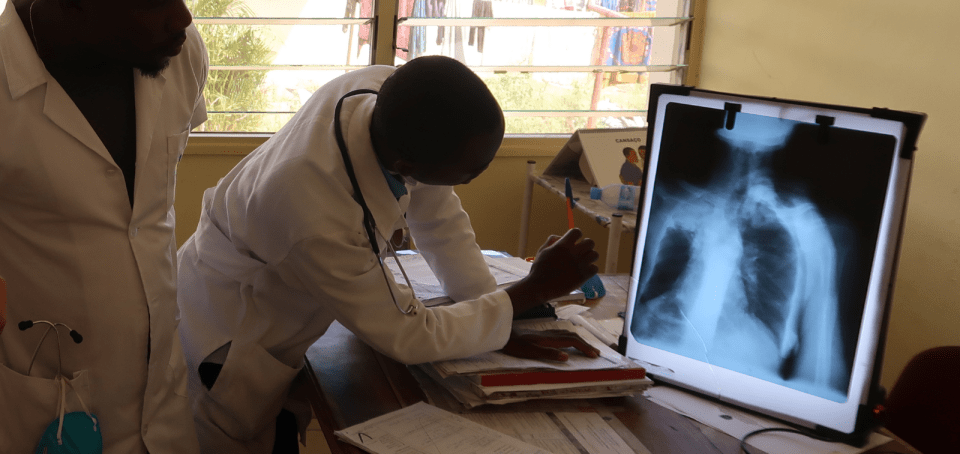
Pulmonary tuberculosis is contagious; in fact, the only type of tuberculosis that is contagious is respiratory. It is transmitted from person to person through infected aerosols; i.e., through the air.
The risk of transmission depends on the following factors: the number of microbes present in the respiratory secretions of the affected person; the extent of lung lesions; and the proximity and duration of exposure to the infected person.
People who live with a patient with pulmonary tuberculosis have a high risk of becoming infected themselves and, once they have been infected, have a probability of at least 5% of becoming ill over the following 5 years, even more so if they are young children.
Because of this risk, the possibility of contagion among contacts of patients with pulmonary tuberculosis is being investigated. People who are close contacts are usually treated to prevent the disease from developing. On the other hand, if there has been contact between the sick person and children, the team will inform you which steps you must follow.
Yes. Given current treatments and the features of the microbes that mostly circulate in our environment, a single, completed standard treatment cures 98.6% of patients permanently. A relapse within 2 years of the end of treatment is experienced by 1.4%; these are cured with a second treatment.
Fortunately, in a developed healthcare environment, the disease is usually diagnosed relatively early and sequelae are few.
The lung is the most frequently affected organ; but today it is rare for tuberculosis to leave sequelae that significantly alter lung function.
The situation is more variable for other forms of clinical infection. Tuberculous meningitis is very rare, and it is still serious. This often leaves significant neurological sequelae.
Renal and osteoarticular involvement can also lead to significant damage of the affected organ.
Although it is rare, tuberculosis of the reproductive organs in women often leads to sterility, despite medical treatment.
Surgery helps to minimise and correct the negative impact of these sequelae.
If patients have no other disorder or complication that requires hospital admission, they can be treated on an outpatient basis from the moment of diagnosis.
If the affected person has pulmonary tuberculosis and is contagious, they will be advised to stay at home and not share enclosed environments with other people during the first two weeks of treatment. Also, during the same period, people who come into contact with a TB patient and the patients themselves are advised to wear a mask.
People who live, or have been in contact, with the patient may go to the hospital's outpatient clinic for the appropriate studies to be done.
If the person has any problem obtaining the medication, it will be provided free of charge at their home by a National Health System Service.
If the person has no disorder or complication that makes it impossible to carry out their professional activity normally and their general status is good, they may return to work 2 weeks after tuberculosis has been effectively treated.
After the first 2 weeks of effective treatment, the person will be able to restart physical activity progressively until normal.
If the patient practises competitive sports, adequate and progressive prior retraining is advisable. The disease will have led to a loss of muscle mass and patients will have been inactive for a long period of time.
Your medical team may recommend avoiding excessive exertion or competitive sport until later in the treatment, especially if you have passed blood with your sputum (haemoptysis), as exertion may precipitate bleeding.
Once the contagious phase has passed (at least 2 weeks of effective treatment), if the person has no other disorder or specific complication and tolerates the medication well, there is no problem in travelling. However, you should check with the medical team beforehand.
When travelling, there are some recommendations to be remembered: ensure your supply of medication; carry a clinical report about the disease; avoid as far as possible places where adequate health care is not possible; and plan your stay so that any medical check-ups you need are not delayed excessively.
There is no special diet to improve the treatment of tuberculosis. One of the common medicines, isoniazid, could interact with products contained in cured or blue cheeses and tuna, so it is better to avoid these foods. However, it is very rare for this to happen.
One of the most serious potentially toxic effects of the medication is inflammation of the liver (hepatitis). The risk of this complication increases with increasing alcohol consumption, so all alcoholic beverages should be avoided.
Generally speaking, a balanced diet is adequate. If the patient's nutritional status is deficient, the medical team may indicate a specific supplement.
If the person has diabetes or some other metabolic disorder, they should take into account the general dietary recommendations appropriate for their disease. Isoniazid causes vitamin B6 to be lost in the urine, so the doctor may decide to prescribe a supplement. You may also be deficient in vitamin D so the team may recommend taking it.
Substantiated information by:

Published: 1 February 2023
Updated: 1 February 2023
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox