Treatment of a Parotid Tumour
After diagnosis, staging of the tumour is performed to determine its extent and whether it has spread to lymph nodes or other areas. Staging is crucial to determining appropriate treatment.
Treatment may vary depending on the type of tumour and its nature (benign or malignant). However, the most common approach is surgery to remove the tumour and, in some cases, additional radiation therapy to kill residual cancer cells. Drug treatment is usually considered in more advanced situations or if the tumour is inoperable.
Treatment is personalised to the needs of each patient, and is based on the recommendations of the medical team after a complete evaluation.
Extended lumpectomy. This is performed with the assistance of a neurostimulator that locates and alerts when working near the facial nerve. If the tumour is highly peripheral, it is removed without dissection of the entire facial nerve.
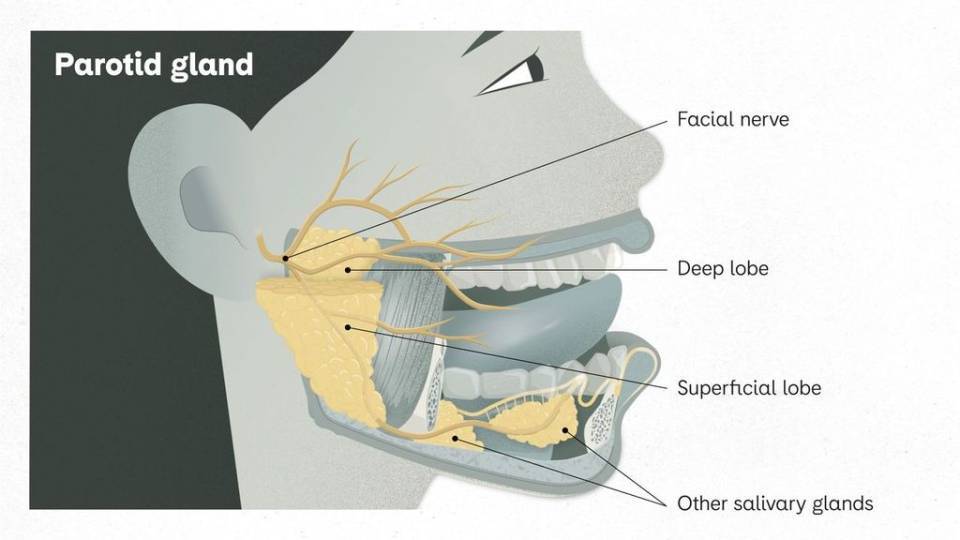
Removal of part of the parotid gland (superficial parotidectomy). This is done when the tumour is in the superficial part (superficial lobe) of the gland, and the part above the facial nerve is removed. The goal is to preserve the function of the facial nerve and gland.
Removal of the entire parotid gland (total parotidectomy). When the tumour is malignant, large or positioned such that partial removal is inappropriate, the affected parotid gland is removed. The aim is to preserve the facial nerve to minimise changes in facial function, but this may vary depending on the extent of the tumour.
Radical removal (radical parotidectomy). This procedure is performed in advanced malignant tumours that have spread to nearby structures, such as nerves or lymph nodes. It involves the removal of the parotid gland (with the facial nerve inside), regional lymph nodes and other affected structures.
Reconstruction techniques. In some cases, especially after a total or radical parotidectomy, reconstructive surgery (immediate or delayed) may be performed to restore facial function and appearance. This may involve tissue transfer, such as a nerve or muscle tissue graft (reconstructive microsurgery), to restore facial nerve function; or static techniques to gain facial symmetry, aesthetically improve the face and reduce functional impact.
It should be noted that the choice of the specific surgical procedure depends on evaluation of the tumour by the medical team, with careful planning to minimise side effects and complications. Parotid surgery should be performed by a surgeon experienced in maxillofacial or in head and neck surgery with reconstructive experience, as preservation of facial nerves and function is a crucial aspect.
After surgery, radiation therapy or facial rehabilitation therapy may be required to achieve a complete recovery and minimise aesthetic and functional sequelae.
Postoperative Indications

Drainage. After surgery, the patient has a drain that remains in place for the first 24-48 hours and is removed before being discharged home.

Stitches. Normally, they are removed after 10-12 days, during a follow-up visit at the hospital.

Incision care. The incision must be kept clean and dry. It should be cleaned with soap and water and the area dried well. Aqueous chlorhexidine can be applied as a disinfectant.

Inflammation. Depending on the patient, a variable degree of inflammation may be experienced in the operated area, which is controlled with compression. The discomfort is usually controlled with conventional anti-inflammatory medication and painkillers.

Diet. During hospital stay, a normal diet is progressively introduced. Once at home, patients should eat foods that do not cause discomfort, with a diet that allows them to chew easily; increasing the texture of the foods as they become better tolerated.

Exercise. Relative rest (sitting with some mobility) is recommended for the first week after the operation, with a progressive return to usual activity after the first postoperative monitoring.

Hygiene. The patient can shower from the first day after surgery.

Medication. Sometimes, the patient needs to follow prophylactic antibiotic treatment a few days after surgery, with anti-inflammatory medication (for 2-3 days after the operation, after meals) and painkillers, to relieve any discomfort.
When should I call the doctor?
If patients experience significant inflammation, redness in the area, fever or worsening in their general condition, the specialist should be consulted.
Non-pharmacological treatment
Non-pharmacological treatment of parotid tumours depends on the nature of the tumour, its staging and individual patient features. The approach to treatment is determined after complete evaluation by a medical team specialising in oncology or head and neck surgery.

Radiotherapy. Radiotherapy uses high-energy radiation to destroy or damage cancer cells. It is used as primary treatment in cases where surgery is not an option or as an adjunctive therapy after surgery, to destroy the remaining cancer cells or prevent their recurrence.

Rehabilitation. After surgery, facial rehabilitation and speech therapy may be necessary to help patients regain facial function and appearance as well as to treat potential complications, such as facial nerve weakness. When nerve reconstruction procedures are performed, combination with subsequent rehabilitation is essential.

Medical monitoring. Regular medical follow-up is essential to monitor tumour progression after treatment and to detect any early recurrence.
Drug treatment
Pharmacotherapy of malignant parotid tumours is not the first line of treatment and is usually used in combination with other therapeutic approaches, such as surgery and radiotherapy; depending on the type of tumour and its staging.
Drug treatment includes the following approaches:

Chemotherapy. Chemotherapy is a treatment that uses drugs to stop or slow down the growth of cancer cells. In the case of malignant parotid tumours, such as squamous cell carcinoma or mucoepidermoid carcinoma, chemotherapy may be an additional option to surgery and radiation therapy. However, this is not the main treatment, as glandular tumours are generally not very sensitive to chemotherapy.

Targeted therapy. Some parotid tumours express certain proteins or markers that can be the target of specific drugs known as targeted therapies. These drugs are designed to block specific signalling pathways that promote tumour growth. Targeted therapy can be used along with other treatments.

Immunotherapy. Immunotherapy uses drugs that stimulate the patient's immune system to kill cancer more effectively. Despite that, it is not a first-line therapy for parotid tumours, with options under investigation to treat certain types of head and neck cancer.
It should be noted that the drug treatment of parotid tumours depends largely on the type of tumour, its staging, the patient's general condition and other individual factors. Treatment decisions are made after a thorough evaluation by an oncological committee made up of the multidisciplinary team that diagnoses, follows up and treats these diseases (specialists in radiology, nuclear medicine, pathological anatomy, oncology and surgery).
Substantiated information by:


Published: 9 May 2024
Updated: 9 May 2024
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox