Cervical cancer treatment
With appropriate treatment, cervical cancer has a high cure rate: the 5‑year survival is over 90% for very early stages and 50–60% in more advanced stages.
Surgery is usually indicated for early-stage tumours measuring less than 4 cm, provided that there is no evidence of lymph node involvement in imaging tests. For larger tumours or when there are signs of lymph node involvement, the treatment of choice is chemoradiotherapy; however, in both situations the lymph nodes are surgically removed and studied so that radiotherapy can be tailored to each patient. The lymph nodes are normally studied using a procedure called a laparoscopy and only the sentinel node, the one closest to the original tumour, is examined in the case of very small tumours (if this node is disease free, it avoids the need for a more extensive study).
Surgery is indicated for cervical cancer in tumours measuring less than 4 cm and that only affect the uterine neck (stage I).

Radical hysterectomy. The surgical removal of the uterus, the parametrium or ligaments that attach the uterus to the pelvic wall (safety margin), the lymph nodes (radical pelvic lymphadenectomy), ovaries and fallopian tubes (this is not compulsory in young women or for small tumours).

Radical trachelectomy. Used to treat early-stage tumours (stage I and less than 2 cm) and in young women who still want to have children. Most of the cervix and parametrium is removed, but the uterine cavity is left intact to preserve its reproductive capacity.

Simple trachelectomy. An even more conservative procedure can be performed on very initial tumours, either all of the cervix is removed or just a cone-shaped portion (cervical conisation).
All of these interventions may be approached by means of an incision in the abdomen, through the vagina, using conventional laparoscopy or robotic surgery.
A more conservative lymph node treatment (sentinel node) can be used for patients with early-stage tumours and some other specific cases. A marker is injected in the tumour to identify which is the first node or lymph node station to receive lymphatic drainage. Selective biopsy of the sentinel node can rule out the need to remove all the lymph nodes when they are not actually affected.

The planning or implementation of the radiation technique usually relies on imaging tests such as MRI or PET to obtain an accurate definition of the area to be irradiated and the appropriate dose. These measures are designed to ensure optimal treatment of the tumour and minimise the amount of radiation applied to healthy tissues.

After external radiotherapy, treatment proceeds with brachytherapy (internal radiotherapy) due to the high doses required to treat cervical cancer and, again, to minimise the exposure of healthy tissues.
In the case of cervical cancer, brachytherapy consists of placing one applicator in the uterus and others around the vagina while under general anaesthesia. In around a third of cases, some small plastic tubes are also inserted in the parametrium to fully optimise the treatment. Brachytherapy is normally planned with the aid of MRI. The procedure is carried out on an inpatient basis and the applicators are usually inserted twice, with a one-week interval between treatments and one night of hospitalisation for each application; alternatively, the applicators may be inserted in a single intervention with four applications of radiation and two days in hospital.
Radiation therapy can also be administered in very advanced cases to alleviate symptoms such as pain or bleeding.

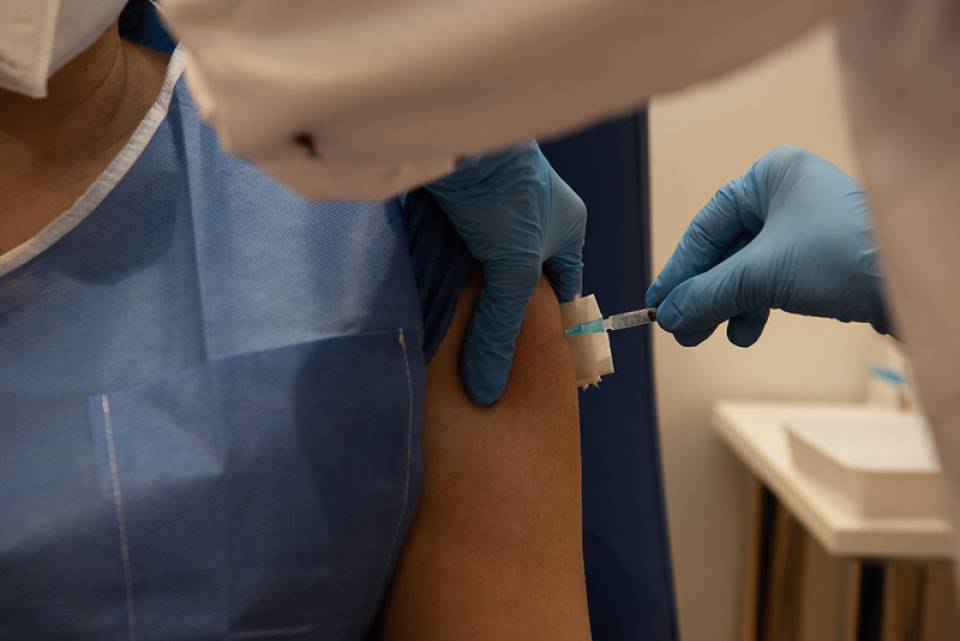
Chemotherapy is a drug-based treatment administered intravenously to reach the entire body. Chemotherapy agents destroy fast-growing cells, so they attack tumour cells when they divide and reproduce.
Chemotherapy may be indicated for cervical cancer at different moments during the illness:
- Preoperative treatment (neoadjuvant treatment). Designed to reduce the size of the tumour before surgical treatment.
- Complementary postoperative treatment in combination with radiotherapy (adjuvant treatment).
- Main treatment in combination with radiotherapy when the disease is localised to a single site, but surgery is contraindicated (chemoradiotherapy).
- Systemic treatment after the development of metastasis (when the cancer spreads to other organs).
To date, the only targeted therapy approved for the treatment of cervical cancer is bevacizumab.
Cervical cancer involves a growth and development process, in the same way as other types of cancer, that results in the formation of new blood vessels leading to the tumour. This ensures that the tumour receives its own nutrient supply required for continued growth.
Bevacizumab is a drug that targets vascular endothelium growth factor (VEGF), a protein that contributes to the formation of the new blood vessels. Consequently, bevacizumab works by blocking the growth of new blood vessels.
Bevacizumab is administered intravenously every 3 weeks in combination with chemotherapy. It tends to produce different side effects from those associated with chemotherapy. The most frequent are hypertension (high blood pressure) and proteinuria (excess proteins in the urine), so patients’ blood pressure and urinalysis test results are monitored during treatment.
Cancer can entail a wide variety of physical problems, but it also produces psychosocial and emotional difficulties. The treatment of cervical cancer, particularly in advanced stages of the disease, must address all of these aspects.
Palliative care is a fundamental part of cervical cancer management, as it improves the quality of life for patients and their relatives and can be beneficial at any point during the treatment of cervical cancer.
Pain is the most habitual symptom and may require several treatment modalities such as the use of analgesics and/or radiotherapy. Bowel obstruction and fistulas are also common problems; palliative surgery may be an option in carefully selected patients.
The most frequent complications of radical surgery are:

Bleeding that requires transfusions.

Damage to neighbouring organs (urinary bladder, ureters, rectum, intestine, blood vessels, nerves) that could require further interventions.

Postoperative infection, pulmonary embolism, lymphoceles or lymphoedema (accumulations of lymph fluid after removing lymph nodes).

Bladder (lack of sensation or urinary incontinence) or rectal dysfunction (constipation).
Chemotherapy acts on cells in the process of division. However, it affects both tumour and healthy cells, which is what causes the symptoms associated with the treatment, known as adverse effects or side effects.
Depending on the specific type of chemotherapy administered, each treatment will cause different side effects. It is very important to learn about them before starting treatment. If you have any questions, you should discuss them with your doctor.
The most frequent acute complications associated with chemotherapy for cervical cancer are:

Alopecia or hair loss. This occurs because chemotherapy agents (in this case paclitaxel) act on –and therefore destroy– hair follicles, which results in hair loss.

Nausea and vomiting. Nowadays, there are some very effective medicines available to prevent these side effects and most patients do not suffer them or they are only mild during treatment.

Low immune system (neutropaenia). This tends to occur 7–10 days after treatment. The chance of infections increases when defences are low, so patients may have symptoms such as fever and/or chills. Talk to the clinical centre if you have any of these symptoms.

Other side effects of chemotherapy are tiredness, loss of appetite, mucositis (the appearance of ulcers inside the mouth, above all on the lips, tongue and throat), constipation or diarrhoea.
The most common chronic complications associated with chemotherapy for cervical cancer are:

Numbness, tingling, increased sensitivity to cold or heat and, in the severest of cases, weakness or difficulty walking (neuropathy). Both paclitaxel and cisplatin, drugs used to treat cervical cancer, can cause damage to nerve endings, primarily in the feet and hands. In most cases these side effects disappear after finishing the treatment, but they can last for a long time in some patients.
Acute complications of radiotherapy
The most commonplace issues are diarrhoea and urinary problems. These can be alleviated with treatment that is generally well tolerated and they tend to disappear within a month. Patients may also suffer from general weakness or nausea, which should be reported to the medical team for management.
Chronic complications of radiotherapy
The most prevalent complication is a bowel movement frequency that varies between constipation and diarrhoea; where necessary, this can often be resolved through dietary measures. In the case of diarrhoea, the customary measures used to relieve this symptom are indicated. A rare complication is the appearance of blood in stools or urine, both of which are treatable side effects. Other even rarer complications are intestinal stenosis and fistulas. If these problems emerge, appropriate steps should be taken to diagnose and treat them.
Substantiated information by:

Published: 21 February 2020
Updated: 21 February 2020
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox