What is a Hysterectomy?
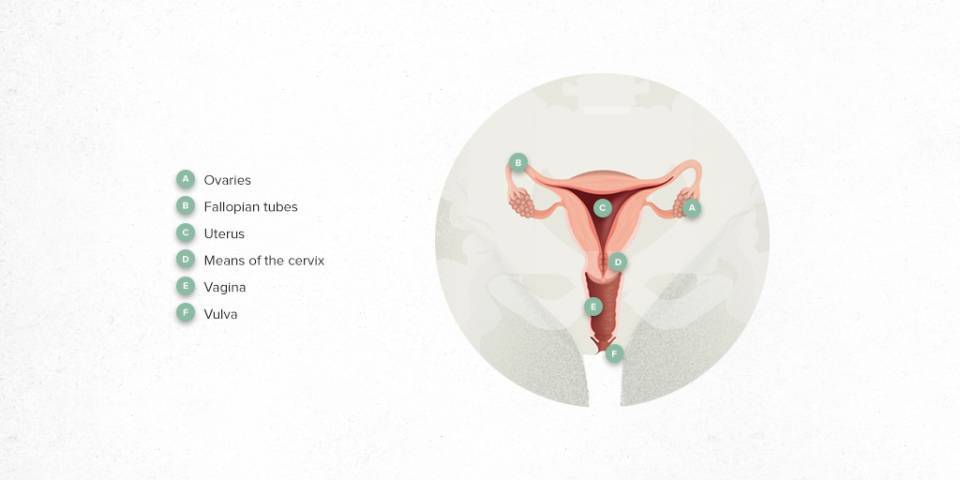
A hysterectomy is a surgical procedure to remove the uterus.
In most cases, the uterus (body and cervix) is completely removed; this is called a total hysterectomy. A subtotal hysterectomy is when the main body of the womb is removed, leaving the cervix in place.
Currently, both fallopian tubes are usually removed (salpingectomy) in conjunction with the hysterectomy procedure.
Performing a hysterectomy does not involve removal of the ovaries. The ovaries may be removed, depending on aspects such as the age of the patient and the presence of associated ovarian pathology.
How it is performed?
A hysterectomy is the most common gynaecological surgical procedure in the world. It can be done via any of the usual access routes in gynaecology, which are:
-
Vaginal hysterectomy: the uterus is removed through the vagina, which leaves no abdominal scars. This is the route of choice and the most common for uterine prolapse surgery (the pelvic floor muscles weaken and no longer adequately support the uterus).
-
Abdominal hysterectomy: access is through the abdomen. There are different modalities of abdominal surgery practised today, which are:
-
Open surgery: this involves a wide, vertical incision in the abdomen, above the pubis and below the navel. This is usually done for women with a large volume uterus or cancer, in some cases.
-
Laparoscopic surgery: a minimally invasive technique in which small incisions are made in the abdominal wall that allow access to a thin tube called a laparoscope. The tube has a camera attached that sends images to a screen. This allows the surgeon to see inside the pelvis.
For this surgery, a pneumoperitoneum is performed; that is, the abdominal cavity is filled with gas (CO₂).
This is the technique used most today, due to the advantages it offers patients: less pain, better recovery, reduced hospitalisation and less risk of complications.
-
Robotic surgery: here, small incisions are also made in the abdominal wall, through which robotic arms are placed that direct the surgical instruments (e.g. scalpel and forceps) inside the pelvis. These arms are remotely controlled by the surgeon.
When is a hysterectomy done?
A hysterectomy is done in cases of benign or malignant gynaecological pathology; that is, where there are malignant tumours (cancer) or other types of diseases.
It is considered the definitive treatment for benign diseases which do not respond to drug treatment or are not well tolerated, especially when the patient has uterine bleeding and pelvic pain. It is also given to patients with no desire for children or uterine preservation.
The main diseases requiring a hysterectomy are:
-
Uterine fibroids (benign tumours): this is the most common indication for a hysterectomy.
-
Endometriosis.
-
Uterine Prolapse.
-
Abnormal Uterine Bleeding.
-
Pelvic pain.
-
Gynaecological cancer: Ovary, endometrium or cervix.
How should you prepare?
This is major surgery; so indications will be given by the nursing, anaesthesia and surgery teams. The preparation procedure for the most common operation consists of:

Preoperative tests: these include a blood test and an autologous blood donation, in case a transfusion is needed.

Electrocardiogram and/or chest x-ray: According to the age of the patient.

Low-residue diet: this is low in fibre, fat and lactose and must be followed for 5 days before entering the operating room.

Fasting: on the day of surgery.
Will I be able to take my medication?
All the patient's usual medication should be maintained until the time of surgery, providing there is no specific indication otherwise from the anaesthesia or gynaecology team.
If the patient has been prescribed a specific gynaecological treatment (generally hormonal) to treat the symptoms that motivate the hysterectomy, this should also be maintained until the day of surgery. After surgery, most hormonal treatments can be suppressed or modified.
What happens during the operation?
Upon arrival in the operating room, the prophylactic antibiotic is given about 30 minutes before the start of the surgery through the line previously placed in the hospital ward.
General anaesthesia is required for an abdominal hysterectomy (open, laparoscopic or robotic); while locoregional anaesthesia (perispinal) can be given for the vaginal route.
Once the anaesthesia is administered, the area where the operation will be performed is disinfected with antiseptic solution. A bladder catheter is inserted that will be removed postoperatively.
Surgery consists of the coagulation and sectioning of the veins, arteries and ligaments that anchor the uterus to the pelvis, so the uterus can be extracted later. It is customary to remove it from the vagina opening; however, depending on the patient characteristics (e.g. vaginal deliveries or age) or if the uterus is very large, extraction can be performed minimally by enlarging the umbilical orifice.
The team performing the operation is usually made up of 3 gynaecologists, an anaesthetist, an anaesthesia nurse, a scrub nurse and a circulating nurse.
How long does it last?
Most laparoscopic abdominal hysterectomies take 60-90 minutes. Vaginal hysterectomies tend to be shorter, around 60 minutes.
However, in calculating the total surgery time, it must be borne in mind that it depends on different factors: the reason for the hysterectomy, if it is associated with other procedures, the uterine volume or other reasons that could increase the surgery time.
What happens after the hysterectomy?
After the surgery, the patients are left in the hospital ward.
After 6-8 hours, they can eat by mouth again, the urinary catheter is removed and gradually they can begin to move.
In general, hospital discharge is 24-48 hours if the surgery has been done vaginally and laparoscopically, and 3-4 days if it has been done through the open abdominal route.
If the patient has an oncological disease or if a highly complex hysterectomy has been carried out, the hospital stay may be longer.
It is customary to advise rest for about 4 weeks. During this time, you should not lift anything heavy, have sexual intercourse or take vaginal douches until the gynaecological control visit, when the healing process will be evaluated.
Remember, most patients do not have their ovaries removed; therefore, the patient will stop menstruating permanently but will continue to have normal hormonal cycles until physiological menopause.
What are the potential complications?
Complications associated with minimally invasive hysterectomy techniques (vaginal and laparoscopic) are low; a hysterectomy is considered a safe procedure with a quick recovery. The most common complications include:

Bleeding which may, in many cases, require an iron supplement to be taken for mild postoperative anaemia. In more severe cases, a transfusion or even a reoperation may be required.

Wound infection.

Dome haematoma (which can be superinfected). Bleeding associated with the healing process of the vagina.

Urine infections.

Injury to neighbouring organs. This would be one of the most serious complications: ureteral, bladder, rectal injuries. Later, fistula complications in the form of vesico-vaginal, recto-vaginal fistula much less frequent.
Substantiated information by:

Published: 14 January 2022
Updated: 14 January 2022
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox