- What is it?
- Causes
- Symptoms
- Risk factors
- Tests and diagnosis
- Treatment
- Life after a disease
- Research lines
- Frequently Asked Questions
-
The disease at the Clínic
- Team and structure
Frequently Asked Questions about Ictus
What is wrong with me?
Most nerve fibres exiting the brain and which control the body's different functions cross over in the neck, and therefore mobility and feeling are affected on the opposite side of the body from where the stroke occurred.
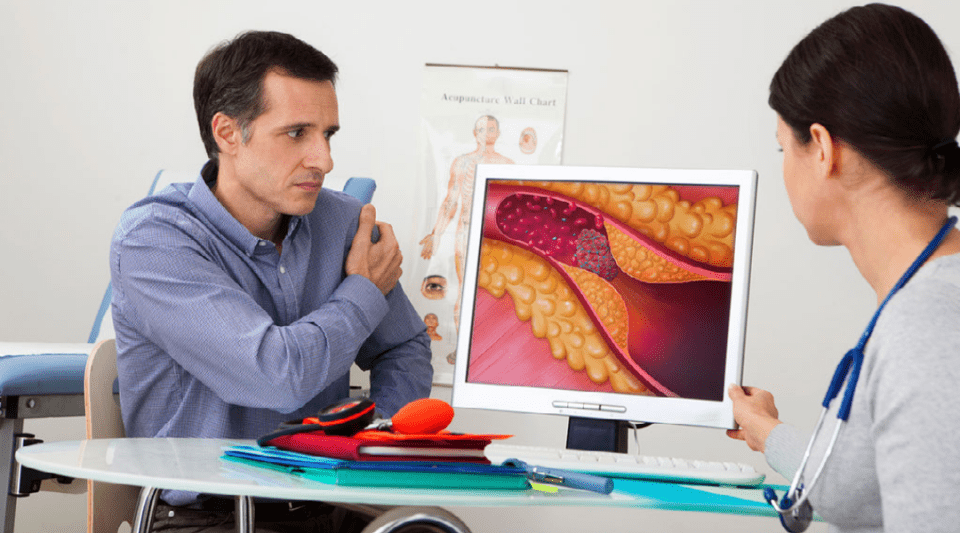
In ischemic strokes, the occlusion of an artery forms by the formation of a thrombus. The presence of said occlusion and the possibility of eliminating it through a drug or intervention is essential, especially in the first hours after the stroke.
In the following days, the fact that the thrombus persists is less critical, and other issues are more relevant: the neurological status of the patient, if complications arise and, the complementary tests' results aimed at finding the cause of the stroke. And choosing the most appropriate preemptive treatment.
Patients who experience numbness or weakness on one side of the body may also notice pain in this zone. This does not mean that the muscles are damaged.
What tests will they do to me?
Computed Tomography is a test that, through the use of X-rays, allows to obtain radiographic images of the interior of the organism in the form of transversal cuts or, if necessary, in the way of three-dimensional images. The CT scan is quick, painless, non-invasive, and accurate. In cases of emergency, you can identify injuries and internal bleeding quickly enough to help save lives.
What treatments are available?
Individuals who have suffered a mild stroke make a practically full recovery. In patients who experienced a moderate or severe stroke, recovery depends on the size and location of the injury and a full recovery is less likely. Your initial progress also helps predict the prognosis; as time passes and you go through the rehabilitation, then any long-term aftereffects which may arise can be identified.
A person who has had a stroke is more likely to suffer another one than the general population.
The risk depends mainly on the cause of the stroke: strokes related to severe arteriosclerosis of the main arteries are more frequent than strokes caused by atrial fibrillation that has created a thrombus in the heart. In any case, if the patient follows a healthy lifestyle and the necessary medication, the risk of suffering a new stroke falls considerably.
The nervous system recovers slowly and so you need to have patience, be persistent and adopt a positive attitude during rehabilitation. Reports have shown that recovery is quicker when it is: started shortly after the stroke; of high intensity; and well structured by healthcare professionals, including physiotherapists, speech therapists and occupational therapists, amongst others.
The amount of vitamin K in your diet could interfere with the effectiveness of the treatment, producing either an excessive or insufficient anticoagulant effect. Vitamin K is mostly found in plant-based foods, particularly dark yellow vegetables or green leafy vegetables (spinach, broccoli, cabbage, endives, asparagus, etc.). These foods are not prohibited, but you should avoid significant changes in your diet that could alter how blood coagulation is regulated.
Typically after a stroke, recommendations are to follow a Mediterranean diet that is rich in nuts and extra virgin olive oil. Olive oil is a source of more vitamin K than other oils but it is healthier in terms of preventing vascular diseases.
Living after a stroke
Patients normally return home when they are minimally independent or require supervision from family members or carers. To minimise the aftereffects you should continue to receive home or outpatient physiotherapy. Depending on the injuries, you may need to readjust some areas of your home (bathroom, entrances, handrails or other safety measures, kitchen utensils, etc.). There are orthopedic specialists who work with patients requiring special neurological care.
Individuals who have suffered a mild stroke make a practically full recovery. In patients who experienced a moderate or severe stroke, recovery depends on the size and location of the injury and a full recovery is less likely. Your initial progress also helps predict the prognosis; as time passes and you go through the rehabilitation, then any long-term aftereffects which may arise can be identified.
Spanish legislation establishes the psychophysical capacities required to drive a vehicle after suffering a transient or recurrent ischaemic attack. You must not drive for the first 6 months following a stroke, or even after a transient ischaemic attack, until you recover. Additionally, you need to obtain a neurological report that confirms that you do not have any long-term injuries. If you are stable, do not suffer any more strokes during the follow-up period and your injuries do not affect your ability to drive, then you should ask your specialist for a report stating this information and undergo an evaluation in an accredited psychometric test centre. Patients who suffer from recurrent ischaemic attacks are prohibited from driving.
After having a stroke, sexuality can be affected by physical factors, emotional changes, and medication. However, with some adjustments, it’s possible to maintain a satisfying sex life. Managing risk factors—such as following a Mediterranean diet, exercising regularly, and stopping smoking—can help improve sexual function. Open communication with your partner and exploring new ways of intimacy adapted to your current needs are also important. If problems like erectile dysfunction or loss of sexual drive persist after 3 to 6 months, it’s recommended to consult a healthcare professional to find appropriate solutions.
It is important to consider several factors before flying after having a stroke. The decision will depend on the patient’s stage of recovery, their neurological stability, any medical complications that may have arisen since the stroke, and whether significant neurological deficits are present. Once the acute phase of the stroke has passed, there are usually no restrictions on flying, whether it’s a short or long-distance trip.
When travelling, it’s important to keep these recommendations in mind:
- Movement and hydration: it is recommended to move around every two hours and stay hydrated.
- Medication: bring all necessary medication and adjust the schedule if crossing time zones.
- Assistance: if you have mobility difficulties, consider travelling with a companion or requesting assistance from the airline.
Can stroke affect sexuality? After having a stroke, sexuality can be affected by physical factors, emotional changes, and medication. However, with some adjustments, it’s possible to maintain a satisfying sex life. Managing risk factors—such as following a Mediterranean diet, exercising regularly, and stopping smoking—can help improve sexual function. Open communication with your partner and exploring new ways of intimacy adapted to your current needs are also important. If problems like erectile dysfunction or loss of sexual drive persist after 3 to 6 months, it’s recommended to consult a healthcare professional to find appropriate solutions.
Post-stroke fatigue is one of the most common sequelae and can be caused by several factors, including the length of hospital stay, neuroinflammation, brain damage, and psychosocial aspects. The fatigue can be physical and/or mental and is not always related to exertion, which can be frustrating and impact your quality of life. It’s important to gradually resume daily activities, adjust rest periods according to your needs, stay socially active, and slowly introduce physical exercise, which can help reduce the feeling of tiredness. If fatigue persists and interferes with recovery, it is advisable to consult a healthcare professional who can help identify possible causes and suggest management strategies, such as physiotherapy, routine adjustments, or psychological support.
Returning to work after a stroke depends on the type and severity of the sequelae, as well as the nature of your job. In patients with mild damage, a leave of 2-3 months is recommended; however every case is different, so the decision should be personalised. It is important to assess both your physical and cognitive capacities, and consider adjusting work hours or tasks if needed. For jobs that involve high levels of stress or physical strain, a gradual return may be more appropriate.
Speak with your doctor and discuss possible workplace adjustments with your employer to ensure a safe and sustainable return.
After a stroke, it is recommended to start or return to exercise gradually, i.e. beginning with low-intensity exercises and slowly increasing the intensity and duration over time. Before starting any high-risk sports or intense exercise programme, it’s important to consult your doctor to make sure it’s safe and suitable for you.
Substantiated information by:




Published: 20 February 2018
Updated: 24 July 2025
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox