Causes of ischaemic stroke or cerebral infarction

Stroke secondary to arteriosclerosis. Arteriosclerosis is chronic inflammation and hardening of the arteries, leading to the accumulation of cholesterol plaques (atheromatous plaques) on artery walls and the increased risk of thrombus formation. Stroke may be the result of a blood clot that forms in either a cerebral artery or any other artery and then travels to the brain. A thrombus (stationary blood clot) can also form in smaller vessels leading to mini-strokes.

Cardioembolic stroke. Cardiac arrhythmias (particularly atrial fibrillation), dilated cardiomyopathy or heart valve abnormalities can produce blood clots inside the heart. The blood clot can travel through the arteries up to the brain; once there, it may block an artery and cause a stroke. Strokes of this type tend to be extensive as blood clots originating in the heart can be very large.

Strokes due to other less common causes like arterial wall rupture or dissection. Rupture of the arterial wall produces coagulation inside the artery which may block circulation and cause a stroke. The burst is usually due to trauma but it can also occur spontaneously.

Cerebral venous thrombosis: although the majority of ischaemic strokes are caused by a blocked artery, blood clots can also form in the brain’s veins. Anything blocking blood’s return from the brain can lead to venous congestion and hinder drainage from the area. Occasionally this may result in a burst blood vessel and brain haemorrhage.

Stroke of unknown origin (cryptogenic stroke). In some cases, even after a complete work-up, the underlying cause of stroke cannot be identified. These are classed as strokes of unknown origin.
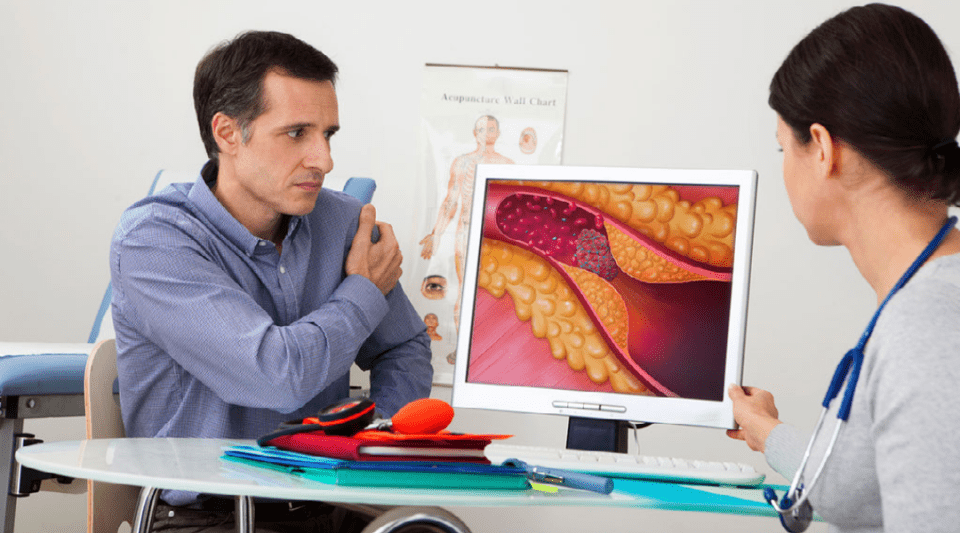
Stroke, cholesterol and statins
High cholesterol (hypercholesterolemia) levels are one of the contributing factors in arteriosclerosis, a chronic artery disease that increases the chance of a blood clot forming in an artery, including those which supply blood to the brain.
Some strokes can be directly related to an artery wall thrombus (blood clot) caused by arteriosclerosis plaque buildup. In such cases it is vital to control all the factors which may accelerate the arteriosclerosis, including cholesterol levels. Medicines known as statins are usually prescribed after arteriosclerosis-associated strokes because they are known to reduce the risk of recurrence.
These drugs not only control cholesterol levels but also produce anti-inflammatory and neuroprotective effects which could explain some of their derived benefits. Whatever the case, it is important to remember that a healthy lifestyle including a good diet and physical exercise help to control cholesterol levels and medicines are only used to complement these measures.
Carotid stenosis
Arteriosclerosis of the carotid arteries, which take blood from the heart and aorta (the main artery exiting the heart) to the cerebral arteries, is one of the primary causes of stroke.
Stroke patients who have significant stenosis or a blockage (typically over 70%) are usually recommended an intervention to treat the stenosis and thus reduce the risk of it causing a recurrent stroke. This intervention may be performed through a surgical technique called an endarterectomy or via an endovascular intervention which dilates the stenosis and inserts a stent (a cylindrical metal mesh).
Carotid stenosis is often identified in patients who have not suffered a stroke, for example during an ultrasound prior to heart surgery or a routine medical examination. Several years ago many of these people with carotid stenosis would have undergone an intervention, but more recent studies have shown that the risk of stroke is much lower when following current treatment for arteriosclerosis (antiplatelet agents, statins, appropriate diet, physical exercise) than in patients who have already suffered a stroke, and so now interventions are not generally indicated in such cases.
Causes of haemorrhagic stroke or brain haemorrhage

Arterial hypertension. High blood pressure (greater than 14/9) is a chronic arterial disease which not only leads to arterial obstruction but also rupture and, therefore, it can cause brain haemorrhages. These haemorrhages tend to occur in deep regions of the brain.

Degenerative processes (cerebral amyloid angiography, CAA). CAA refers to a process in which a substance called amyloid is deposited in arteries. It is more commonly observed in elderly patients and causes cognitive impairment and haemorrhage in areas close to the brain’s surface.

Haemorrhages secondary to brain blood vessel (cerebrovascular) malformations. Although less frequent, intracranial haemorrhages can be caused by the rupture of abnormal blood vessels.
Brain aneurysms
Brain aneurysms occur when cerebral arteries with weak walls dilate. Generally they do not produce any symptoms but if they burst they can cause a subarachnoid haemorrhage – heavy bleeding inside the brain which has a high mortality rate and often produces severe sequelae due to brain damage.
When faced with subarachnoid haemorrhaging, the aneurysm should be repaired either by an endovascular intervention or through surgery to ensure the aneurysm does not bleed again.
However, brain aneurysms are increasingly detected by chance during brain CT or MRI scans conducted for other reasons. In such cases, aneurysms should be treated to prevent subarachnoid haemorrhage whenever the risk of bleeding is greater than the risk posed by intervening on the aneurysm. The most important factor for determining the potential risk of an aneurysm bursting is its size, those larger than 7 mm present significantly more risk.
Other determining factors include the risk associated with the aneurysm’s location (those situated in arteries toward the back of the brain are more likely to burst), patient gender (risk is greater in women) and age (although the risk increases with age, young people have a greater accumulated risk of rupture occurring throughout their lifetime).
Regardless of whether the aneurysm is to be treated or not, factors that could lead to a burst should be controlled, the most important risks being high blood pressure and tobacco use.
Patent foramen ovale
The foramen ovale is a hole, usually very small, that communicates the left and right chambers of the heart. This hole occurs naturally in developing foetuses and closes shortly after birth; however, when it remains partially open, as is the case in over 1 in 4 people, it is called patent foramen ovale.
Patent foramen ovale is predominantly an asymptomatic condition and does not normally require any corrective interventions.
Patent foramen ovale is relevant in strokes because blood clots that form in a vein and which would not normally reach the cerebral arteries may do so via this hole in the heart, this is known as a paradoxical embolism.
Therefore, in strokes known to be due to a venous thrombosis, the cause of the clot is studied and an anticoagulant treatment is often prescribed. Attempts are also made to close the patent foramen ovale, which is generally achieved through an interventional procedure (accessing the heart along the blood vessels).
Patent foramen ovale are usually discovered while studying a stroke of unknown origin; nevertheless, this finding is not a definitive sign that patent foramen ovale is responsible for the stroke as over a quarter of the population have this unclosed hole in their hearts. While the decision about treatment must take into consideration all of the individual factors for each patient, intervention on the hole is not generally indicated in these cases because the risk of recurrent stroke associated with a patent foramen ovale is very low. However, the intervention could be beneficial in young patients with a large oval area who have had a stroke and in whom they have ruled out the reduction of stroke causes.
Substantiated information by:




Published: 20 February 2018
Updated: 27 December 2022
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox