LDL cholesterol, also known as ‘bad’ cholesterol, is one of the main risk factors for developing cardiovascular diseases. In patients with a history, such as of heart attack, reducing this type of cholesterol with intensive drug treatment is essential to prevent the appearance of new cardiovascular episodes and reduce mortality.
A study led by IDIBAPS-HOSPITAL CLÍNIC and the Barcelona Esquerra Primary Health Care Consortium (CAPSBE) has analysed data from almost 2,000 patients who had suffered a heart attack, reviewing their LDL cholesterol levels and the medications prescribed to lower them. The results show that only one third of patients manage to keep their cholesterol under the levels recommended by medical guidelines. In addition, women and older people observably tend to receive less intensive treatments, which lead to them having worse control of their cholesterol levels.
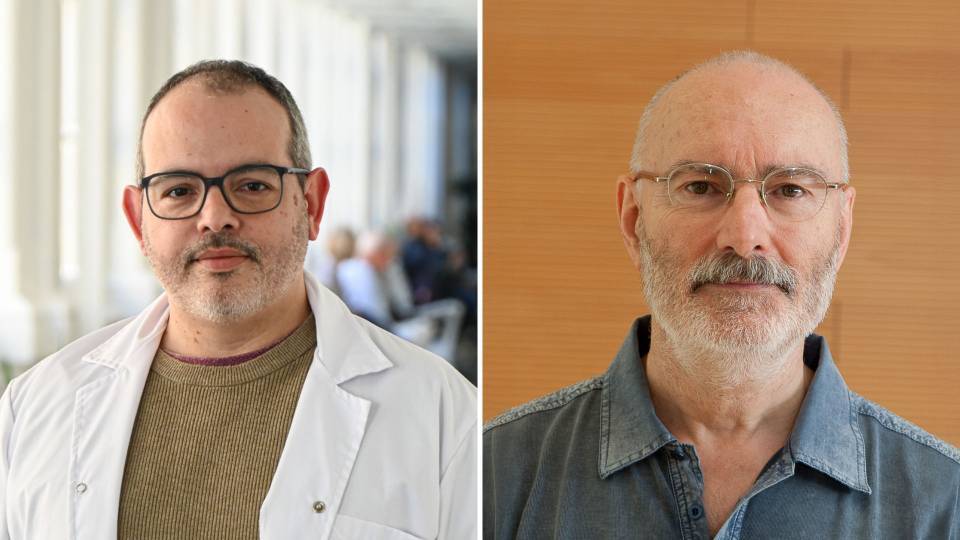
According to Luis González de Paz, attached to CAPSBE and the IDIBAPS Primary healthcare transversal research group, and one the study’s researchers, these results indicate that special attention must be paid to gender and age inequalities, especially in those who already have a cardiovascular history and who require more intensive monitoring and treatment.
The difficulty of lowering cholesterol levels
Data published in the British Journal of General Practice Open reveal that only 35% of the patients studied reach levels below 70 mg/dl of LDL cholesterol, as recommended in old clinical guidelines, and only 12% manage to reduce it to 55 mg/dl, the level currently recommended for these high-risk patients.
To reduce ‘bad’ cholesterol, the guidelines advise changing lifestyle habits (such as quitting smoking, increasing physical activity and improving diet) and often recommend starting treatment with high-intensity statins, which effectively lower cholesterol.
‘Though there are clear protocols on intensive cholesterol treatment, we have observed that most patients used drugs at low doses’, says Dr Núria Sánchez-Ruano, a family physician at CAPSBE and a researcher involved in the study. ‘This indicates that despite receiving the prescription, we’re not using it, and we still have a long way to go to improve these results’.
Gender bias in treatment
Regarding gender differences, the study shows that women are 10% less likely to receive intensive statin treatment compared to men, even where they have higher cholesterol levels.
‘This result could reflect a stereotype that only links cardiovascular diseases to men, forgetting that women also suffer from them. Furthermore, the tradition of a medicine focused from a male perspective could be perpetuating these inequalities in treatment’, González de Paz explains.
Ageism in healthcare
The results show age-based inequality: older patients receive less intensive treatments than younger patients. As such, the probability of receiving very high intensity treatment at 34 years of age is 50%, while at 65 years of age it falls to 21%.
‘This could be related to the perception that intensive treatments are less suitable for the elderly, even though clinical guidelines recommend administering them whenever there are no contraindications’, Sánchez-Ruano explains. These inequalities highlight a broader problem exacerbated by the ageing of the population: ageism, the misperception that older people are considered less suitable for certain treatments.