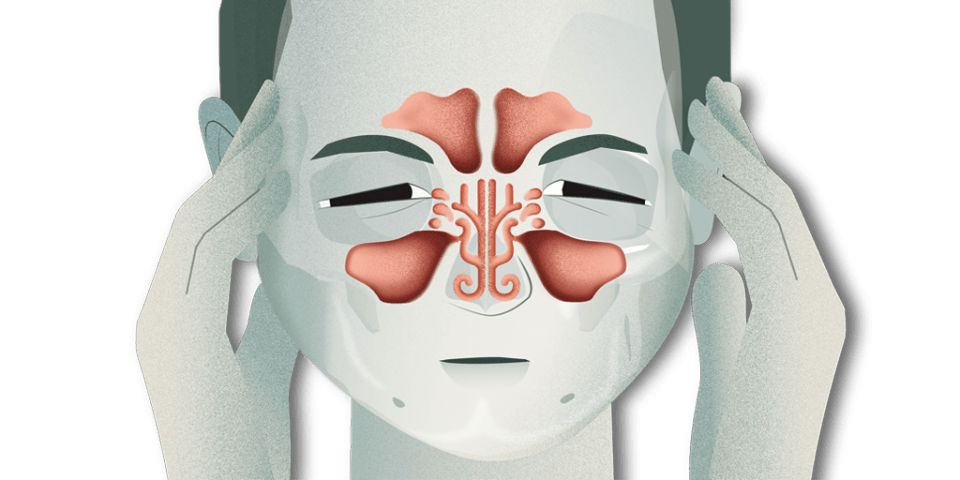
Chronic rhinosinusitis with nasal polyps (NP) is a subtype of chronic rhinosinusitis with a high prevalence, affecting between 2% and 4% of the population. This disease has a negative impact on quality of life and also has a high socio-economic cost. It is a chronic condition with episodes of worsening and is often recurrent in spite of medical or surgical treatment.
Current medical treatment options continue to be limited. Only intranasal corticosteroids (INCs), oral corticosteroids, antibiotics and antileukotrienes have shown efficacy in clinical trials.
Current clinical guidelines recommend both INCs and nasal irrigations with saline solutions as initial therapies. It has been shown that INCs reduce the size of nasal polyps while also improving patients’ symptoms and quality of life.
Current clinical guidelines are based on the observable characteristics or features (phenotypes) of patients with chronic rhinosinusitis. There is still no consensus on the different biomarkers of sinusitis (endotypes). In other words, no specific molecules or manifestations, whether clinical, endoscopic, laboratory or imaging tests, have been identified that would allow a more personalised diagnosis of this disease.
Several studies have been carried out to search for specific rhinosinusitis biomarkers, both in the blood and in the polyp tissue, but they were unable to pinpoint the best ones. Much remains to be studied, as these determinations must be sufficiently specific.
Monoclonal antibodies: a new biological therapy
In recent research, multiple studies have proven the effectiveness of using monoclonal antibodies as a form of precision medicine in sinusitis with polyps. These antibodies are biological drugs that primarily act by interfering at different points in the inflammatory response.
Clinical trials have been carried out with the drugs omalizumab (IgE), mepolizumab (IL-5), reslizumab (IL-5) and dupilumab (IL4 α). Other monoclonal antibodies that could be applied to the treatment of NP due to their mechanism of action, but for which there is still insufficient scientific evidence, include benralizumab (Il-5α), ligelizumab (IgE), lebrikizumab (IL-13), tralokinumab (IL-13), AMG 282 (IL-33) and AMG 157 (thymic stromal lymphoprotein, TSLP).
Lectins, proteins similar to some types of immunoglobulin, are also potential treatments. Laboratory studies have shown that the release of pro-inflammatory mediators is reduced when these proteins are bound.
Under current European regulations, patients with rhinosinusitis who may be candidates for these drugs must meet three or more of the following criteria: an impaired quality of life, significant loss of smell, needing to take systemic corticosteroids, or having polyps despite surgery, among others.
This research aims to achieve the greatest control of the disease in the shortest time possible, as well as more personalised treatment of chronic rhinosinusitis with polyps, based on each patient’s clinical, cellular and blood marker characteristics.
Author: Dr Cristóbal Langdon, otolaryngologist, Institute of Medical and Surgical Specialisations at Hospital Clínic