Intestinal microbiota resist treatments such as chemotherapy or antibiotics and, after a disruption of this balance, are normally able to return to their normal state after a period of time. However, should this balance not be restored, it is an ideal opportunity for opportunistic pathogenic microorganisms to grow and settle in the intestine, causing an infection. This is the case with Clostridioides difficile infection, the main cause of infectious diarrhoea in hospitalised patients in the world, with recurrence rates of 20-30%. For these patients, one of the therapeutic options gaining more and more traction is to restore this community of microorganisms via Faecal Microbiota Transplantation (FMT).
Why is intestinal microbiota so important?
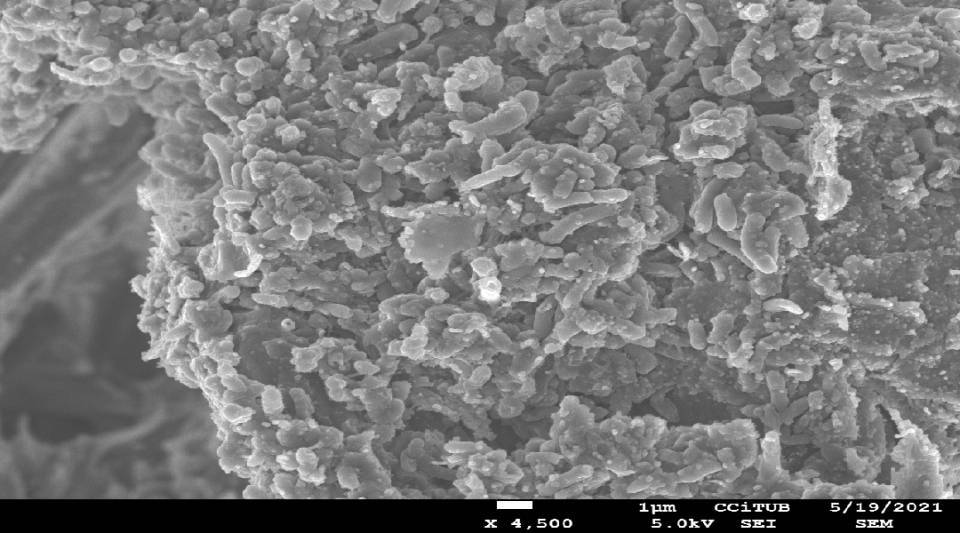
Intestinal microbiota consists of millions of microorganisms comprising over 1,000 different species. This set of microorganisms is present at birth and evolves according to a person's lifestyle, environment and diet, and is considered as a second "fingerprint". It has essential functions in the body; among them, breaking down and obtaining nutrients from food in the diet. It provides vitamins and substances involved in the metabolism and also has a fundamental role in regulating the immune system.
What does Faecal Microbiota Transplantation (FMT) consist of?
This procedure consists of obtaining intestinal microbiota from the faeces of a healthy donor and transferring it to the colon of a patient to restore the latter’s flora. The procedure is generally performed by colonoscopy or nasogastric tube using the faeces of a relative or close friend of the patient; however, this is increasingly changing towards oral administration by capsules with the faeces of universal donors being used. And, although FMT may seem a modern treatment, this is not so. The procedure was used in the 4th century in China as a treatment in serious cases of food poisoning and diarrhoea and was known as "yellow soup". It is included in the first Chinese medicine manual called Zhou Hou Bei Ji Fang, by the sage, Ge Hong.
Currently, FMT is recognised in different clinical guidelines as a treatment of choice for recurrent C. difficile infection, with an efficacy greater than 90%. In addition, there are more than 200 active clinical trials around the world studying the use of FMT for various pathologies. From inflammatory bowel diseases, urinary infection, decolonisation of multiresistant bacteria, metabolic diseases such as diabetes and obesity, neurological diseases and even behavioural disorders.
What limits the use of Faecal Microbiota Transplantation (FMT)?
The availability of prepared treatments for faecal transplantation depends on access to healthy stool donors to provide these samples. Exhaustive screening protocols to ensure the safety of the recipient patient are carried out, which reduces the number of valid donors to a minority. To solve this problem, Stool Banks have emerged; these are institutions that select healthy donors and store processed samples they make available to hospitals and health centres.
There is a lack of awareness on the part of the general population about faeces donation. Unfortunately, there is a taboo in our society around this issue which means people are not generally aware of it. As a result, and unlike blood donation, it means many potential donors do not come forward. Thus, emphasising the importance of intestinal microbiota as a treatment for so many pathologies may make the population reflect and result in an upturn of altruistic faeces donors.
Author: Andrea Aira Gómez, microbiologist and predoctoral researcher at the Microbiology Unit, Hospital Clínic, Barcelona.