Restoring circulation after an ischaemic stroke is of key importance to preserving the function of the affected area of the brain and to ensuring that patients recover with as few sequelae as possible. A study coordinated by researchers from the Hospital Clínic-IDIBAPS and published in the journal JAMA shows that the administration of a treatment after intervention to trap the thrombus significantly improves the patients’ prognosis. This study will represent a paradigm shift in the treatment of ischaemic stroke.
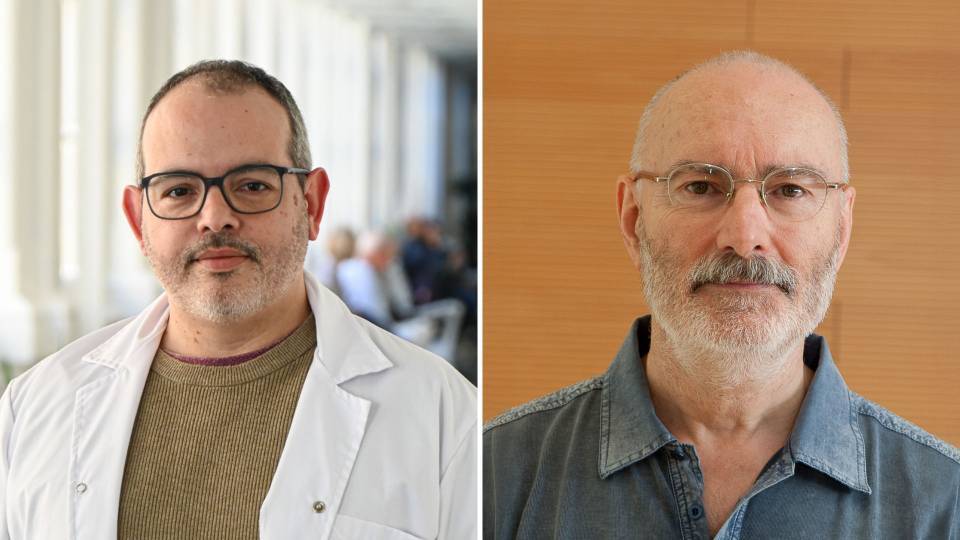
Dr. Ángel Chamorro, head of the Cerebrovascular Pathology Unit and of the IDIPABS Cerebrovascular Disease research group designed and coordinated the study and is presenting the results at the International Stroke Conference in New Orleans. The first author of the article and coordinator of the trial at the Hospital Clínic was Dr. Arturo Renú, from the same team.
The study received funding from La Marató de TV3 in 2016, which was devoted to strokes and traumatic spinal cord and brain injuries, and involved all tertiary hospitals in Catalonia dedicated to stroke care: Hospital Clínic, Hospital Universitari Germans Trias i Pujol, Hospital Universitari de Girona Dr. Josep Trueta, Hospital de Bellvitge, Hospital de la Santa Creu i Sant Pau, Hospital del Mar, and Hospital de la Vall d'Hebron.
An ischaemic stroke, which occurs when a blood vessel carrying blood to the brain becomes blocked, represents 85% of all stroke cases. When there is a lack of blood supply, the function of the affected part of the brain may be temporarily or permanently impaired.
During the first few hours after a stroke, it is crucial to act quickly, since on average two million neurons die every minute. Therefore, treatments to restore blood flow should be used up to 24 hours after the stroke.
Restoring circulation, the key in an ischaemic stroke
Mechanical thrombectomy is a type of treatment that consists of introducing a catheter into the femoral artery through which a stent is moved forward into the blocked artery in order to trap the thrombus in the stent’s mesh and remove it from the circulatory system. This is an extremely complex procedure that is only carried out in tertiary hospitals with highly qualified professionals.
"In almost 80% of cases we manage to get the blood circulating normally again, but we have observed that after three months the percentage of people who are completely free of sequelae is 27%", explains Ángel Chamorro. “We are much more effective at restoring normal circulation than the clinical efficacy we observe", he adds.
This difference in percentages is evidence that the brain tissue close to the formation of the thrombus will die, even if the blood circulates again with apparent normality.
What the study suggests is that, although the main artery is open, cerebral microcirculation is affected. “This microcirculation is obstructed. It is as if we were opening a motorway but keeping the exits closed”, says Dr. Chamorro.
Treating what you cannot see
The microcirculation is below the diagnostic level of cerebral arteriogram that is used to see the reperfusion after the mechanical thrombectomy. In order to restore it, researchers considered administering a fibrinolytic drug, which enhances the thrombus dissolution and helps restore the blood flow, after the thrombectomy is carried out. “With this approach, we treat what we cannot see but we know is there”, explains Arturo Renú, head of the trial at the Hospital Clínic.
The study published in the journal JAMA involved 121 patients treated at tertiary stroke hospitals in Catalonia. One group of patients was given the fibrinolytic treatment (r-tPA) after the mechanical thrombectomy, and the other group received a placebo after the same procedure.
The results of the study show that, by administering this treatment, the patient’s chances of making an excellent recovery with no sequelae three months after the procedure are increased by up to 59%. “We are giving a drug after the treatment that used to be given before the treatment. So, first, we restore the circulation in the main artery and then we give the drug, which is effective at breaking up the smaller thrombi", explains Dr. Renú.
"Despite the enormous difficulties caused by the COVID-19 pandemic, this clinical trial has obtained extraordinary results in the treatment of ischaemic stroke, which will change the clinical guidelines for its treatment", says Arturo Renú.
"This work represents a paradigm shift in the treatment of the disease worldwide", points out Ángel Chamorro. With the results obtained, moreover, the satisfaction is twofold, since we carried out the study thanks to funding from La Marató de TV3: the donations made by the public have yielded a direct benefit for society, with an intervention that clearly improves patient recovery”, he concludes.
Study reference:
Effect of intraarterial alteplase following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke: the CHOICE randomized trial
Arturo Renú, Mònica Millán, Luis San Román Manzanera, Jordi Blasco, Joan Marti-Fabregas, Mikel Terceño, Sergio Amaro, Joaquin Serena, Xabier Urra, Carlos Laredo, Roger Barranco-Pons, Pol Camps-Renom, Federico Xavier Zarco Contreras, Laura Oleaga, Pere Cardona, Carlos Hernan Castaño Duque, Juan Macho, Elisa Cuadrado-Godía, Elio Vivas, Antonio López-Rueda, Leopoldo Guimaraens, Anna Ramos-Pachón, Jaume Roquer, Marian Muchada, Alejandro Tomasello, Antoni Davalos, Ferran Torres, Ángel Chamorro; for the CHOICE Investigators
JAMA. Published online February 10, 2022. doi:10.1001/jama.2022.1645