- What is it?
- Team and structure
What is Coronary Angioplasty with Stenting?
Coronary angioplasty with stenting is one of the interventional coronary procedures used to widen heart arteries obstructed by the accumulation of fat, cholesterol or other substances. To prevent recurrence at the same site, a stent is also implanted inside the artery. The stent is a cylindrical metal mesh that adheres to the walls of the arteries and keeps them open so that blood flow is adequate. The narrowing of the arteries is detected beforehand by a coronary angiography.
Interventional Cardiology Coronary Procedures
Interventional coronary procedures are used to treat blockages of heart arteries caused by a build-up of fat, cholesterol or other substances, known as atheromatous plaque. This build-up causes a type of heart disease known as atherosclerosis. To gain access to the coronary arteries during an operation, very fine tubes, called catheters, are inserted through an artery or vein in the leg or arm. This is different to open surgery, which requires opening the chest to reach the heart.
Interventional coronary cardiology procedures consist of performing two tests, coronary angiography and angioplasty.
Coronary angiography is used to assess whether the coronary arteries, which supply blood to the heart, function normally or not. It checks if the arteries have been narrowed by cholesterol plaque and if they might cause angina or a heart attack. Angioplasty treats strictures, diagnosed in coronary angiography, by inserting a stent.
What is Coronary Angiography?
Coronary angiography consists of inserting a plastic tube or catheter, about 2 mm in diameter, through an artery in the wrist to reach the arteries of the heart. The procedure is performed under local anaesthetic with a contrast injected to visualise the state of the arteries.
If the procedure cannot be performed via the wrist, it can be done through a larger diameter artery via the groin. This route entails no greater pain or additional discomfort compared to performing it via the wrist. The only difference is that the patient must rest for about 24 hours.

In coronary angiography, the arteries are visualised as smooth tubes. Compromised, narrower or even totally obstructed segments can be observed (green arrow in the image). If the coronary angiography shows one or more significantly obstructed arteries, angioplasty with stent insertion is performed.
What is Coronary Angioplasty with Stenting?
Coronary angioplasty consists of inserting a catheter of about 2.5 mm diameter with a balloon inside. This is inflated and thus dilates and corrects the narrowing or stenosis of the blood vessel. The angioplasty catheter can be inserted by the same route as the coronary angiography catheter; another entry point is not required.
When the balloon is inflated, the atheromatous plaque breaks up and the narrowing is corrected. After the artery has been dilated by the balloon, a metal mesh a few millimetres in diameter and length, called a stent, is implanted where the narrowing had occurred. This acts as a metallic support for the artery to help keep it open and reduce the acute risk of re-obstruction.
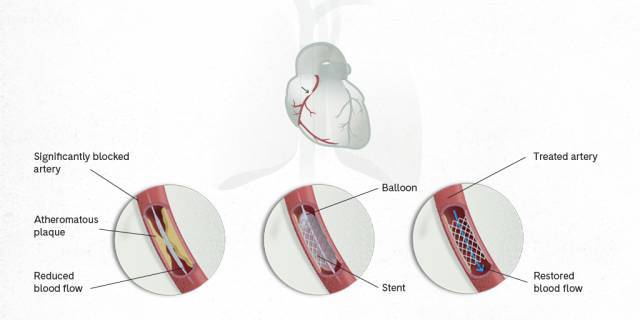
The stent is mounted on the balloon exterior. When the balloon is inflated, the stent also expands. This is left inside when the balloon is withdrawn, keeping the artery open. The stent remains inside the artery indefinitely and normal blood flow is restored.
When does a Coronary Angioplasty need to be performed?
Coronary angioplasty is necessary in two different clinical situations:
- Acute situation. When a patient has chest pain at rest, this is a sign of a heart (myocardial) infarction. In this case, an urgent coronary angioplasty is performed to reopen the artery that has been acutely blocked by the formation of a blood clot.
- Chronic situation. When a patient has chest pain on exertion, due to atherosclerotic plaque formation obstructing an artery in the heart which cannot be controlled by medication.
How should I prepare for the procedure?
A few days beforehand, a nursing professional contacts the patient to inform him about the steps to be taken, the date and place of admission, fasting time, the medication to be taken before the procedure and any medication to be discontinued. You will also be asked you if you are allergic to iodine contrast or any other substance, and given the guidelines to be followed if this is the case. You will also be informed about any part of the body to be shaved and whether it is necessary to remove headphones or glasses.
Where is the procedure performed?
The procedure will be performed at the Cardiac Haemodynamics Unit, in a room similar to an operating theatre.
Who performs the procedure?
Specialists in cardiology, specifically in cardiac haemodynamics, as well as nursing professionals will perform the procedure. These professionals have received specific training in the use of catheters, contrast media and fluoroscopy; as well as in balloon angioplasty and coronary artery stent implantation techniques.
How long does the procedure take?
It takes approximately 40 minutes.
What will I feel during the procedure?
During the coronary angiography, the patient will notice the injection of local anaesthesia and an initial stinging sensation followed by tingling. You will also feel that "something" is going through your arm, as well as a sensation of heat in that arm. During the test, you may experience palpitations, a sensation of chest pain or shortness of breath and even nausea and/or vomiting due to the radiological contrast used.
If an angioplasty is performed, the medical and nursing staff will inform the patient of the different sensations he may experience. However, access to the artery and stent insertion are generally painless.
What happens after the procedure?
Once the procedure is over, the patient will stay overnight in a room in the cardiology ward.
- If the procedure is performed via the wrist, the patient will be able to move immediately, although the arm must be kept still until the compression bandage is removed. This bandage is usually removed 3 hours after the end of the procedure.
- If the procedure is performed via the groin, the patient should rest for 12 hours and avoid moving or bending the leg for the first 6 hours. The bandage is removed after 12 hours and the patient will be able to move if there is no bleeding or other contraindication.
The ward nursing staff should be informed if any of the following is experienced:
- Pain or discomfort in the chest.
- A feeling of wetness or blood in the bandage.
- Pain in the wrist or leg near the entry point.
The hospital discharge report states that there must be no exertion of the arm or leg operated upon for 48 hours, to prevent bleeding or bruising after the operation.
What are possible complications?
The most common complications are:
- Allergy to one of the substances used. Allergic reactions, mostly due to the radiological contrast used, are frequent. In general, these are mild reactions that are easy to treat, with serious reactions being very rare.
- Hypotension or slowing of the heart rate, usually temporary, in 2-3% of cases.
- Local vascular complications (at the puncture site), such as bruising or excessive bleeding (in 2% of catheterisations).
Other rare complications are:
- Severe arrhythmias, requiring electric shock or a pacemaker.
- Cerebrovascular accidents, such as a stroke.
- Acute myocardial infarction
- Impaired kidney functioning.
The aforementioned complications have a very low mortality rate of less than 0.1%.
Stent placement complications
Apart from complications that can occur during or immediately after catheterisation, there are also those due to implantation of a stent in a heart artery. At 9-12 months, the artery may become blocked again where the stent has been located. This process, called restenosis, has an incidence of 3-5% and mostly occurs in complex patients.
It is also important to remember that the patient has to take antiplatelet medication after a coronary stent is fitted. This ensures the blood is kept fluid and liquid and prevents a stent thrombosis from occurring during the healing process of the artery (about 6-12 months).
Does a specific lifestyle have to be followed?
To reduce the risk of having a cardiac event, such as a heart attack, you should keep the different cardiovascular risk factors under control and lead a life with healthy habits.
Risk factors fall into two categories:
- Non-modifiable. Non-modifiable risk factors are age and being male or female.
- Modifiable. These are factors which medical professionals and especially patients can act on, with changes in lifestyle or medication to keep them under control and prevent or reduce the risk of developing heart disease. These modifiable risk factors are high blood pressure, high cholesterol, smoking, diabetes, obesity and a sedentary lifestyle. In fact, in some cases, maintaining a healthy lifestyle alone can control risk factors without having to take medication.
However, you need to abstain from smoking and drinking alcohol; take exercise (walking 30 minutes/day); follow a low-fat diet, rich in fruit and vegetables (especially avoiding sausages, red meat, soft drinks, refined sugars, butter, margarines, fast food and snacks); and maintain optimal weight. If it is not possible to control these cardiovascular risk factors despite leading a healthy lifestyle, there are currently highly effective drugs available, such as antihypertensives and statins.
Related contents
Substantiated information by:


Published: 25 July 2023
Updated: 25 July 2023
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox
