Schizophrenia symptoms
Schizophrenia is an extraordinarily complex disease because it combines a multitude of symptoms. To assist in its identification, the symptoms have been divided into four large subgroups:

positive symptoms,

negative symptoms,

emotional or affective symptoms, and

cognitive symptoms.
It is important to explain that the terms positive or negative do not mean that the symptoms are good or bad. Psychiatrists use the concept of positive psychiatry to refer to something that was not present in the past, whereas the term negative psychiatry defines the loss of a previously acquired ability or trait.
It is worth highlighting that patients do not present all of these symptoms at the same time. In fact, patients never experience most of them and many only manifest fleetingly and temporarily during periods of crisis or imbalance. On the other hand, some symptoms (particularly negative symptoms, but also others) present chronically and are resistant to treatments, so the patient and their carers must learn to live with them.
What are positive symptoms?
The positive (or psychotic or reality distortion) symptoms of schizophrenia can be grouped into three types:
- Delusions. These are false beliefs. Patients present a specific conviction that does not follow logical thinking.
- Hallucinations. These are sensory errors. Patients hear voices or see things in the absence of a genuine stimulus. There are as many different types of hallucinations as there are sensory organs: auditory, visual, tactile, etc.
- Behavioural disorganisation. Disorganisation can be observed in both the patient’s thoughts and their behaviour. Disorganised thinking is evident when a patient’s speech becomes less comprehensible or when they repeatedly iterate the same idea, sentence or even a single syllable. This tendency sometimes evolves and the person’s ideas do not follow a semantic order (agrammatism) or logical argument (disaggregated or slow thinking), which leads to unintelligible or incoherent speech. When the disorganisation affects behaviour, patients may be restless and even become agitated or violent for no apparent cause. This behaviour can sometimes accelerate to such an extent that it paradoxically leads to a state of absolute immobility, with rigid arms and legs, called catatonia.
For the family and people close to the patient, these positive symptoms often constitute the first warning sign announcing the disease’s presence and the reason why they visit a specialist for the first time, although the patient may have already been suffering other less notable symptoms for weeks or months.
We must not forget that, although they create disbelief and amazement in those around them when they first announce their experiences, the patient’s delusions and hallucinations are absolutely real for them; they are totally convinced they exist and therefore act according to their distorted reality.
Due to the presence of these symptoms and their absolute conviction of the reality in which they are living, patients behave according to these influences. This type of behaviour is often what first warns the family about the condition, even when the patient has still not explained what is happening to them. People around the patient will notice that they:
- become more suspicious of others,
- believe many things happening around them are their concern (self-referentiality),
- become very vigilant or fearful, as if expecting to be attacked at any moment,
- are distrusting, they avoid contact with others and tend to isolate themselves out of fear, and
- often speak to themselves or listen to very loud music to block out the annoying voices inside their heads.
What are negative symptoms?
Negative symptoms are associated with:
- reduced ability to feel or experience emotions,
- a loss of motivation,
- difficulty to enjoy themselves, and
- a reduction in verbal expression.
These symptoms frequently appear before the positive symptoms, but as they are usually less evident, they may go unnoticed during the early stages of the disease. Their presence determines the long-term prognosis for patients because they have a much greater impact on adaptive capacity than other symptoms.
What are the affective symptoms of schizophrenia?
As a general rule, patients with schizophrenia will also present depressive symptoms. Two situations are typically associated with the appearance of depressive symptoms in schizophrenics. The first is during the onset of the disease, when patients experience the initial psychotic symptoms and the strangeness of the world around them. The second, more common situation occurs after the delusional or hallucinatory (reality distortion) symptoms have remitted, when the patient is diagnosed and becomes aware of their condition and the consequences that they must overcome.
What are cognitive symptoms?
Patients with schizophrenia present decreased capacities in certain aspects or cognitive domains, such as attention span, working memory or executive functions, those which allow us to plan, anticipate and order our actions. In one way or another, these patients may manifest a loss of some of these intellectual capacities, which is why, for a long time, schizophrenia was known as “early dementia”. Specialists can determine the degree of dysfunction, which varies greatly between patients, by means of neuropsychological tests designed to measure what are known as mental, superior or cognitive functions.
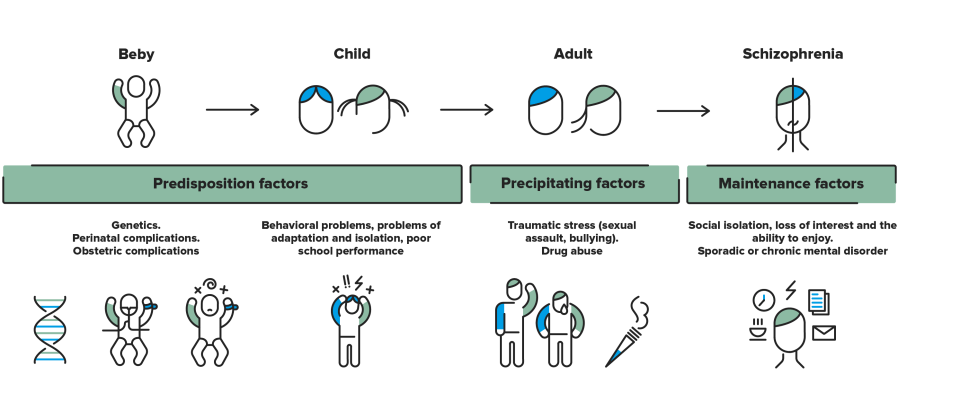
Disease onset and progression
Given the large variation in how the disease manifests, there is no unique clinical course. The disorder may arise in different ways, according to various pathological routes, and so each case is different.
The most exemplary case is that of slow onset. Weeks or months pass before somebody finally notices that something strange is happening. The initial (prodromal) symptoms are similar to other mental illnesses, such as depression, a tendency towards isolation, decreased workplace or academic performance, disregard for personal care, disinterest in social relationships, etc. Other warning symptoms progressively start to become evident, e.g., irritability, suspicious nature, hostility and strange explanations for their own behaviour, demonstrating that the affected person is suffering from more than just a period of sadness.
Once installed, the disease is characterised by the patient’s distorted perception of reality, including delusions and hallucinations. In fact, it is not uncommon for months (or even years) to pass in which the patient has adapted to their distorted reality and they only display a few occasional and unexplainable idiosyncrasies before being diagnosed and treated.
Substantiated information by:


Published: 20 February 2018
Updated: 30 November 2022
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox