Frequently asked questions about Multiple Myeloma
Maybe at some point during the course of the disease you may feel some pain, particularly in your bones, but do not hesitate to visit your medical team as they will help you attain the best possible control over this symptom.
Yes. There is a type called smouldering or indolent myeloma. Patients present altered levels of antibodies in blood and plasma cells in the bone marrow, as do all patients with myeloma, but in this case they do not present any of the symptoms or blood test and skeletal survey abnormalities associated with symptomatic myeloma. These patients are at risk of developing symptoms of myeloma in the future and must be studied and monitored specifically according to the perceived risk. A much more common antibody abnormality is known as monoclonal gammopathy of undetermined significance (MGUS), which is often observed among the healthy population, particularly those aged 60 or over. People with MGUS present a small change in the amount of the protein in the blood while their bone marrow plasma cell count is normal and they do not present any symptoms. This group of patients should also be studied and monitored in function of the corresponding haematological findings since they have a slightly greater risk of developing myeloma than people who do not carry this antibody.
No. Multiple myeloma is not a genetic disorder and the vast majority of cases do not present any specific genetic predisposition. The relatives of myeloma patients do not need to undergo any tests or a genetic study to rule out the presence of abnormal proteins.
Younger patients without any contraindications and who respond well to the initial treatment can receive an autologous transplant (high-dose chemotherapy followed by administration of the patient’s own, previously harvested, bone marrow stem cells) is an early treatment option. An allogeneic transplant (with bone marrow stem cells harvested from someone other than the patient) is no longer considered the standard treatment for multiple myeloma due to the associated complications. This treatment option may be offered in a few select cases, depending on the centre, prognosis, patient’s age, response to other treatments and the likelihood of finding a bone marrow donor.
Research developments made at centres specialising in multiple myeloma are shared across the globe and so haematological treatments offer the same or similar guarantees.
Many treatments can be administered on an outpatient basis, but in some cases they may require a hospital stay.
Biological therapy or immunotherapy is a treatment designed to stimulate the body’s immune system to act against cancer cells. It is generally administered by intravenous infusion.
Which patients are eligible for immunotherapy treatment?
It uses proteins (antibodies) to attack other proteins found on the surface of tumour cells, hence it is a more tumour-specific treatment. In the case of multiple myeloma, antibodies have been developed to attack proteins expressed at the plasma cell surface. They tend to produce less severe and different adverse effects from conventional chemotherapy.
The doctor will request analytical tests (blood tests, urine tests, bone marrow aspiration) and sometimes imaging tests (X-rays, CT scans, MRIs) during treatment to help assess the course of the disease throughout each cycle and at the end of the treatment.
Treatments known as complementary or alternative therapies (e.g., homeopathy, acupuncture, relaxation techniques, massage, Reiki, etc.) can have beneficial effects, such as helping to treat the symptoms caused by the disease or treatment. In any case, you must always discuss any alternative therapies with your doctor before starting them and they can never impede or interfere with the specific treatment planned by your medical team.
Many multiple myeloma treatments, including the new agents that act specifically against malignant plasma cells, do not explicitly cause a significant degree of hair loss. However, in some cases, patients may suffer hair loss if they have to receive a bone marrow transplant.
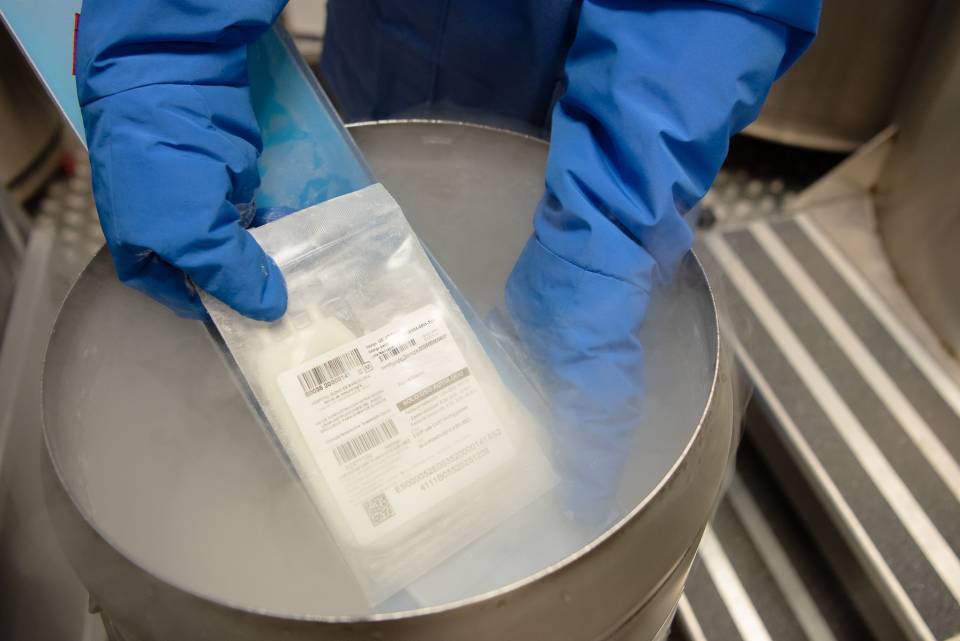
There are currently two types of bone marrow transplant; autologous (autotransplants) and allogeneic transplants – the former uses the patient’s own stem cells, while the latter uses someone else’s stem cells. The choice of transplant depends on the patient’s response to treatment and their age. In both types of transplant the stem cells are administered as if they were any other intravenous medication, just like a packed red blood cell or whole blood transfusion, or similar.
Some aspects of your everyday lifestyle will be restricted for a few days after a bone marrow transplant; as the weeks go by, you can return to your normal lifestyle, depending on each patient’s tolerance.
It is very important that you look after your skin while being treated as many treatments can produce toxicity. You should use soft shower gels and apply moisturising cream every day. Avoid exposure to the sun and use high sun protection factor sunscreens.
Fever is a very common symptom after receiving treatment. You should visit your healthcare team and must not take any medications until indicated to do so by a doctor. Patients often need to visit emergencies services and/or outpatient care if it is a high fever or presents with associated complications.
It is vital that you maintain good oral hygiene and clean your teeth after every meal with a soft-bristled toothbrush to prevent mouth sores. You should complement your oral hygiene with mouthwashes, alternating between a physiological solution and a sodium bicarbonate solution (1 cup of water + 1 teaspoon of bicarbonate).
Depending on which treatment you receive, they may insert a catheter in one of your veins. There are two types of catheter, a central venous catheter and a peripherally inserted central catheter. Your healthcare team will tell you everything you need to know about their insertion and everyday life while wearing one.
Patients undergo regular check-ups after the treatment, including laboratory tests on blood and urine samples, X-rays and analytical tests, which are all assessed during the appointment with your doctor.
Deciding whether or not to tell your children, grandchildren or other family members is a very personal choice. It can depend on age, circumstances and the type of treatment. The family may decide it is better not to tell the children about such information. However, as a general rule, patients are advised to explain it to them as they are particularly sensitive to change.
This depends on your occupation and the acute complications arising from the disease or its treatment. Patients who receive a bone marrow transplant must stop working at least temporarily while they undergo the procedure.
Substantiated information by:


Published: 20 February 2018
Updated: 20 February 2018
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox