Multiple myeloma treatment
It is vital patients understand the information provided by their medical team so they may make an accurate analysis and assessment of the treatment options that best suit their day-to-day life, age and occupation.

Healthy, balanced diet. Spread out over four meals per day. Use simple cooking techniques – steam, bake and grill – and avoid fried or heavily seasoned foods.

Stay well-hydrated. Drink at least 1.5–2 L of fluids per day (water, fruit juices, infusions, etc.).

Evitar el consumo de alcohol.

Practice gentle exercise on a daily basis, outdoors if possible.

Take part in leisure activities, with family or friends where possible.

Adopting a positive attitude helps overcome the process better.

Relaxation techniques tend to help patients maintain their emotional stability throughout the course of the disease. Try not to worry too much because stress and anxiety do not help the process.
Hasta hace pocos años los tratamientos para controlar el mieloma eran la quimioterapia, los esteroides (glucocorticoides), las terapias con dosis altas y el transplante autólogo (con las propias células madre de médula ósea). Desde hace unos años se han introducido nuevos tratamientos que están desplazando a la quimioterapia, o bien incorporándose a ella. Estos medicamentos incluyen la talidomida y sus derivados como la lenalidomida y la pomalidomida.
La introducción del bortezomib es un avance muy importante en el tratamiento del mieloma, con una nueva familia de fármacos llamada inhibidores de la proteosoma, que funciona de manera diferente a la talidomida.
También existen nuevos fármacos de esta familia como carfilzomib e ixazomib. Cada vez más hay nuevos fármacos para esta enfermedad, incluyendo anticuerpos monoclonales contra las células malignas, que se van incorporando a las diferentes etapas de la enfermedad.
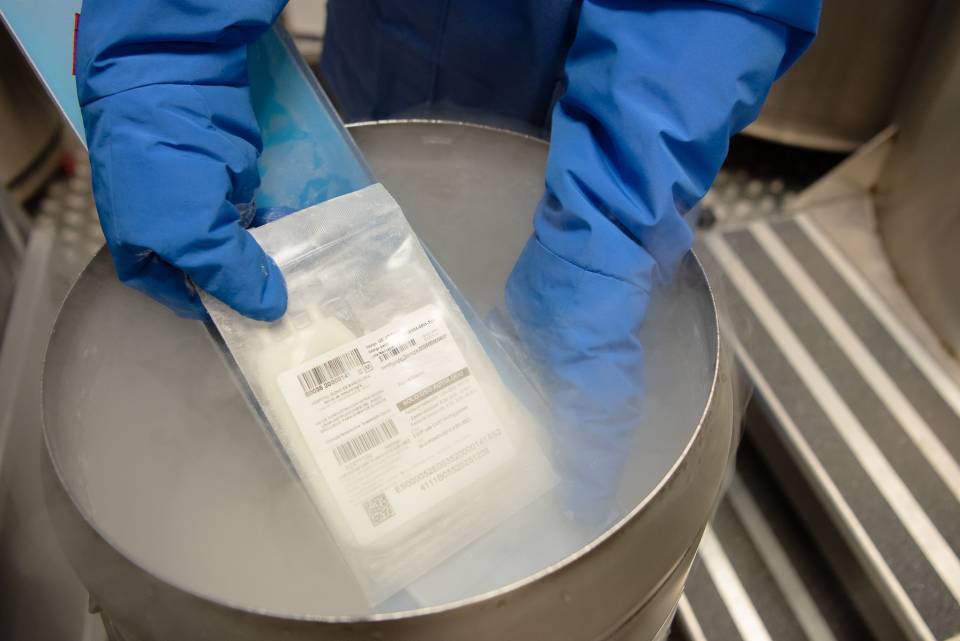
An autologous stem cell transplant forms part of the initial treatment in most multiple myeloma patients under the age of 65–70 years. The patient’s own stem cells are collected in this type of transplant.
In this procedure patients receive several treatment cycles involving a combination of drugs to destroy as many malignant cells as possible and so that the stem cells can be separated and extracted. They are then administered very high doses of chemotherapy and their own stem cells, which were harvested and stored previously, are intravenously infused.
To prevent complications in the period between stem cell infusion and bone marrow recovery, patients may require blood transfusions and antibiotics until their blood counts return to normal.
Finally, the disease is assessed to determine the degree of response obtained and whether or not any additional treatments are required after the transplant.
Although other treatments are available for multiple myeloma, chemotherapy is one of the most common. It is generally administered intravenously, but in some cases it may be taken orally.
Chemotherapy inhibits the growth of cells in the process of division. It affects both tumour and healthy cells which is what causes the adverse effects or side effects associated with the treatment.
Chemotherapy may be administered in combination with other treatments, for example immunotherapy. The number of cycles mainly depends on the patient’s age, the tumour stage and their overall state of health. Various tests are conducted after each chemotherapy cycle to evaluate the treatment’s effectiveness.
Before starting treatment, or after the first dose of chemotherapy, a central venous catheter (CVC) needs to be inserted to simplify the administration of medicines and to avoid damaging peripheral veins. CVCs are inserted in an operating room using local anaesthetic; the procedure does not require an overnight stay.
You must wear this catheter throughout the treatment. Your oncologist and doctor will decide when it should be removed by taking into account the initial diagnosis and prognostic factors at the start of treatment, which could mean you need to wear the device for up to 12 months.
The catheter should be checked 3 months after completing chemotherapy and the last administration of chemotherapy drugs. This check-up should be repeated every 3 months after finishing the treatment. If a PICC type central catheter is inserted, then it can be removed on the same day as the last dose of chemotherapy.

Fatigue. This is one of the most common treatment-related complications. Discuss it with your doctor because there are several options available to treat the causes and help you feel better.

Response associated with a low blood cell count. The lack of red blood cells produces low levels of haemoglobin in blood; this subsequently causes anaemia leading to fatigue and weakness. A low white blood cell count increases the susceptibility to infections, while a low platelet count may mean the patient bruises and bleeds more easily.

Side effects. Certain drugs, such as thalidomide and bortezomib, present special complications as they may damage nerves in the hands and feet (neuropathy).
Palliative treatment is the normal option when the disease cannot be totally eliminated. It is designed to relieve the symptoms of multiple myeloma and improve the patient’s quality of life.
Substantiated information by:


Published: 20 February 2018
Updated: 20 February 2018
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox