- What is it?
- Risk factors
- Symptoms
- Diagnosis
- Treatment
- Living with the disease
- Research
- Frequently asked questions
Tests for diagnosing Dry Eye
There are diagnostic tests common to dry eye syndrome due to lack of aqueous secretion and evaporative dry eye syndrome.
Evaluation of the stability of the tear film

Tear break-up-time (TBUT). After instilling fluorescein and using a slit lamp with the cobalt blue filter, it is observed how long it takes for the tear film to break from the last blink. Values less than 10 seconds after the instillation of one drop of fluorescein or values less than 7 seconds after the instillation of 5 ml with a pipette, are indicative of dry eye syndrome. This is an invasive method due to the application of fluorescein that can alter the measurement.

Non-invasive tear break-up-time (NIBUT). The time it takes in distorting the lines of a reticule projected onto the cornea since the last blink. There are currently several methods for performing this. Values less than 15 seconds are indicative of dry eye syndrome.
Evaluation of tear osmolarity

Osmometer. The TearLab test is easy to use in the clinic with tears, and the results are immediate. The normal values are 308 mOsm/L or less. It is a good test for severe dry eye syndromes, but not so much for mild ones. It can show a wide variability between the two eyes; a variability of more than 8 mOsm/L between the two eyes is characteristic of dry eye syndrome.
Evaluation of inflammation of the eye surface

The InflammaDry method detects the matrix metalloproteinase (MMP) enzymes, which are increased in dry eye syndrome. It is easy to perform and the results are obtained in 10 minutes. It has a sensitivity of 85% and a specificity of 94%.

HLA-DR inflammatory markers can be detected using impression cytology. Other markers are Th1, Th17, or ICAM-1 from the tear. However, these tests are only performed in clinical trials and not in daily practice.
Evaluation of eye surface damage

Fluorescein corneal stain. The fluorescein detects if there are any changes between the intercellular junctions of the cornea and the conjunctiva. Using the slit lamp, the cornea stain is seen with a cobalt blue filter, and the conjunctiva stain with the yellow-green filter. A superficial punctate cornea or conjunctiva is observed (superficial punctate keratitis) in the patient with dry eye syndrome, which can be more or less classified according to the Oxford scale (0-5).

Conjunctiva stain with lissamine green. The lissamine green stains the conjunctiva that is not adequately covered by the mucin layer of the tear film. The most used grading system is that of van Bijsterveld (0-9).
Evaluation of the neurosensory changes

Corneal sensitivity. The instability of the tear film in dry eye syndrome can damage the corneal and conjunctival nerves, and decrease corneal and conjunctival sensitivity. There are several test to measure this sensitivity: the corner of a paper tissue, the Cochet-Bonnet or CRCERT-Belmonte anaesthesiometer.
Aqueous-deficient Dry Eye Syndrome tests
Evaluation of tear volume

Schirmer test. It can be done without anaesthesia (Schirmer 1, measures the baseline and reflex secretions), or with anaesthesia (Schirmer baseline secretion, measures baseline secretion). After placing filter paper strips in the lower temporal tarsal conjunctiva, wait 5 minutes. The moistened area of the paper is measured in millimetres. Less than 10 mm is considered as abnormal.
Evaluation of the height of the tear meniscus

The height of the tear meniscus is measured in millimetres. This measurement is currently made with specialised equipment that analyses the eye surface. They are specific and reproducible and can be used for comparison between different visits by the same patient in order to evaluate a treatment. A decrease in the tear meniscus height is suggestive of an aqueous deficient dry eye syndrome.
Evaporative Dry Eye Syndrome Tests

The thickness of the lipid layer. Is measured using an interferometer. The quality level of the lipid layer can be estimated based on the colour pattern. This measurement is currently carried out with special equipment.

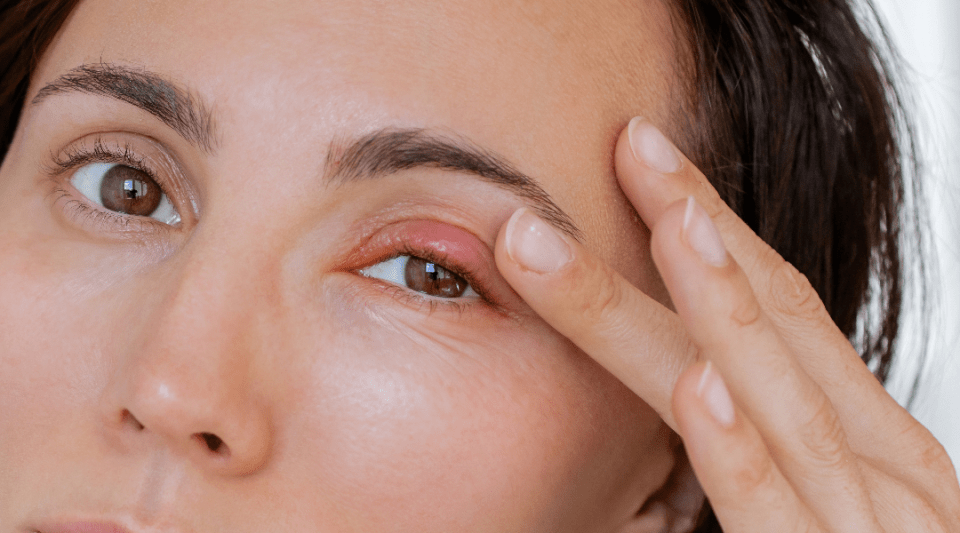
Evaluation of the free eyelid margin. This is done squeezing the edge of the eyelid with the finger, with a cotton swab, or with a “Meibomian gland evaluator” (marketed). There is a scale depending on the type of secretion obtained: 0- clear secretion, normal; 1- turbid secretion; 2- granular secretion, turbidity with whitish-greyish or yellow particles; 3- like toothpaste, difficult to squeeze, comes out like a stopper or a thread.

Meibography. It analyses the characteristics of the Meibomian glands, which included the quantity, the length, the distortion, the thickness, or the atrophy, in both the upper eyelid and lower eyelid. This measurement is currently carried out with special equipment.
Substantiated information by:

Published: 23 May 2019
Updated: 23 May 2019
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox
Dry Eye Syndrome related news
30 November 2023
What are the most common eyelid diseases?
16 October 2023