Although information is still limited, up to now there is no evidence of a higher infection rate of COVID-19 or a more serious disease progression in people with HIV compared to HIV negative people. Some case series of patients with HIV who have had COVID-19 have been published, including the first cases treated at Hospital Clínic, published by the journal Lancet HIV. Furthermore, both the European AIDS Clinical Society and the AIDS Study Group in Spain have issued preliminary statements on this matter.
Current evidence indicates that the risk of developing a serious case of COVID-19 increases with age, being male and with chronic medical problems, such as cardiovascular disease, chronic lung disease and diabetes. These characteristics are currently very common amongst those living with HIV in Europe, as a large number of these patients are now over 50 years of age. It is essential to keep those living with HIV up-to-date with vaccines against influenza and pneumococcus, above all as we approach winter, when SARS-CoV2 and influenza may circulate at the same time. Giving up smoking is also a very positive step to prevent associated problems.
T CD4 cells are the immune system cells infected by HIV. Patients with a low T CD4 cell count (<200/µl), or those not receiving antiretroviral treatment, are considered at risk of suffering more serious infections in general, although this has not yet been observed with COVID-19. Nevertheless, more observation time and a larger number of patients are needed to confirm this. On the other hand, COVID-19 tends to produce an overall decrease in total lymphocytes. This should be assessed in people with HIV to decide whether it is necessary to prescribe prophylaxis for Pneumocystis jiroveci, a fungus that can cause pneumonia in immunosuppressed people, as well as for other opportunistic infections.
In terms of preventative measures, the current guidelines for the general population that aim to reduce the risk of contagion should be followed. Furthermore, it is important for these patients to be especially aware of the appearance of possible COVID symptoms.
Although studies are under way, for now there is no clear evidence that any antiretroviral drug used for treating or preventing HIV protects against SARS-CoV infection. A clinical trial carried out in China with the antiretroviral Lopinavir/ritonavir showed no benefits when administered to patients with serious pneumonia caused by SARS-CoV. A current study designed by the national AIDS programme, which will be carried out on healthcare staff, will try to answer whether TDF-FTC, another antiretroviral drug, offers any kind of protection against SARS-CoV. As such, until there is more information available, there is no evidence to justify changing regular antiretroviral treatment to treat or prevent SARS-CoV infection.
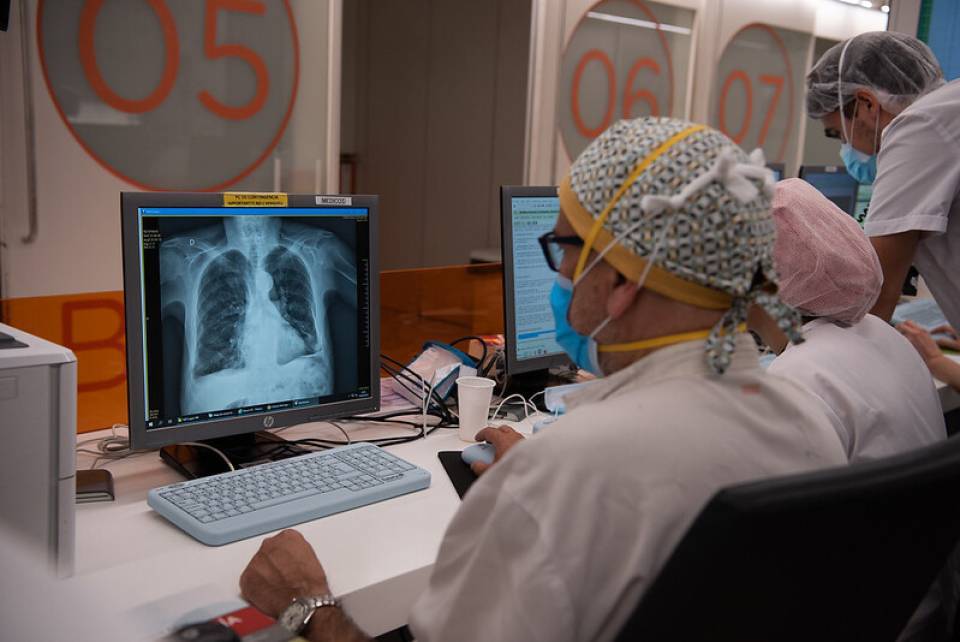
Finally, one of the measures that is being applied universally to reduce the risk of contagion for patients with HIV is substituting in-person visits with telephone consultations. This has been done, above all, for patients who receive antiretrovirals chronically, who would be more exposed to the virus due to regularly visiting a hospital. Of course, an in-person consultation will be conducted when necessary. The development of the COVID pandemic will progressively outline what the future method of consultation will be for people with HIV, in order to give them the best care possible at the lowest risk.
Authors: Dr Juan Ambrosioni, infectious disease specialist, and Dr Josep Mallolas, head of the HIV/AIDS Unit at Hospital Clínic.