Type 2 diabetes (DM2) and obesity are closely linked. A study conducted by researchers from CIBERDEM and IDIBAPS has demonstrated that the absence of the protease BACE2 (β-site APP-cleaving enzyme 2), a possible target for Alzheimer’s disease and DM2, aggravates the metabolic phenotype in mice fed with an obesogenic high-fat diet.
Also participating in the study, led by Joan-Marc Servitja and Anna Novials, from the IDIBAPS Pathogenesis and Prevention of Diabetes research group, were Mario Vallejo’s team from the Alberto Sols Biomedical Research Institute, CSIC-UAM, and the IDIBAPS Neuronal Control of Metabolism group, headed by Marc Claret. The lead author is Daniela Díaz-Catalán, currently in the group of Endocrine disorders: crosstalk between molecular, metabolic and therapeutic determinants of IDIBAPS.
The BACE1 and BACE2 proteins belong to the same family of proteases which cleave membrane-bound peptides. BACE1 is expressed in various tissues, including the brain, where it cleaves the amyloid precursor protein (APP), which initiates the formation of the β-amyloid peptides present in plaques in the brains of patients with Alzheimer’s disease. For this reason, the pharmacological suppression of BACE1 has been proposed as a therapeutic strategy for the treatment of Alzheimer’s. In contrast, BACE2 is found in greater abundance in the pancreatic islets, where it suppresses the secretion of insulin of pancreatic beta cells.
Prior studies by the group demonstrated that the absence of BACE2 led to recovery of the secretion of insulin affected by the toxic effect of over-expression of the human amylin hormone in beta cells. These results led researchers to consider the possibility that the suppression of BACE2 could be a new strategy for the treatment of DM2. For this, however, it was necessary to check the possible consequences of the absence of BACE2 on regulation of the metabolism. For this purpose, a high-fat diet, which induces alterations in the metabolism, was administered to two groups of mice. The results indicated that those rodents with a BACE2 deficiency gained more weight than the unmodified mice in the control group. This effect was preceded by a greater intake of food and an alteration in the inhibitory signals of insulin and of leptin in the hypothalamus. Furthermore, the BACE2-suppressed mice presented higher blood insulin levels and greater diet-induced insulin resistance, evident before the appearance of obesity.
In summary, this study shows that suppression of BACE2 leads to a greater increase in body weight, hyperphagia, hyperinsulinemia and resistance to insulin in mice fed with an obesogenic diet. This finding poses the need to reconsider the use of BACE2 inhibitors for the treatment of diabetes, as well as the use of BACE1 inhibitors, for the treatment of Alzheimer’s disease, since the majority of said drugs lack selectivity and can also inhibit the activity of BACE2.
This work was funded by the Carlos III Health Institute, co-funded by the European Regional Development Fund (ERDF; European Union, A Way) and by CIBERDEM.
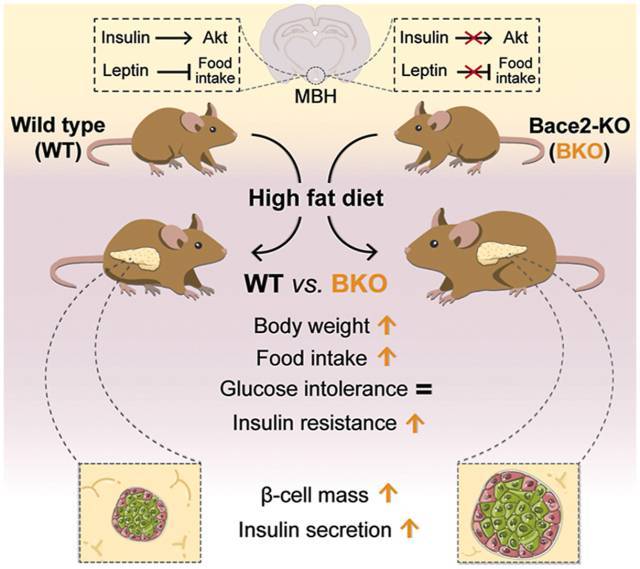
Graphical abstract of the main findings
Reference article
Díaz-Catalán D, Alcarraz-Vizán G, Castaño C, de Pablo S, Rodríguez-Comas J, Fernández-Pérez A, Vallejo M, Ramírez S, Claret M, Parrizas M, Novials A, Servitja JM. BACE2 suppression in mice aggravates the adverse metabolic consequences of an obesogenic diet. Mol. Metab.;53:101251 (2021). doi: 10.1016/j.molmet.2021.101251.
https://www.sciencedirect.com/science/article/pii/S221287782100096X?via%3Dihub