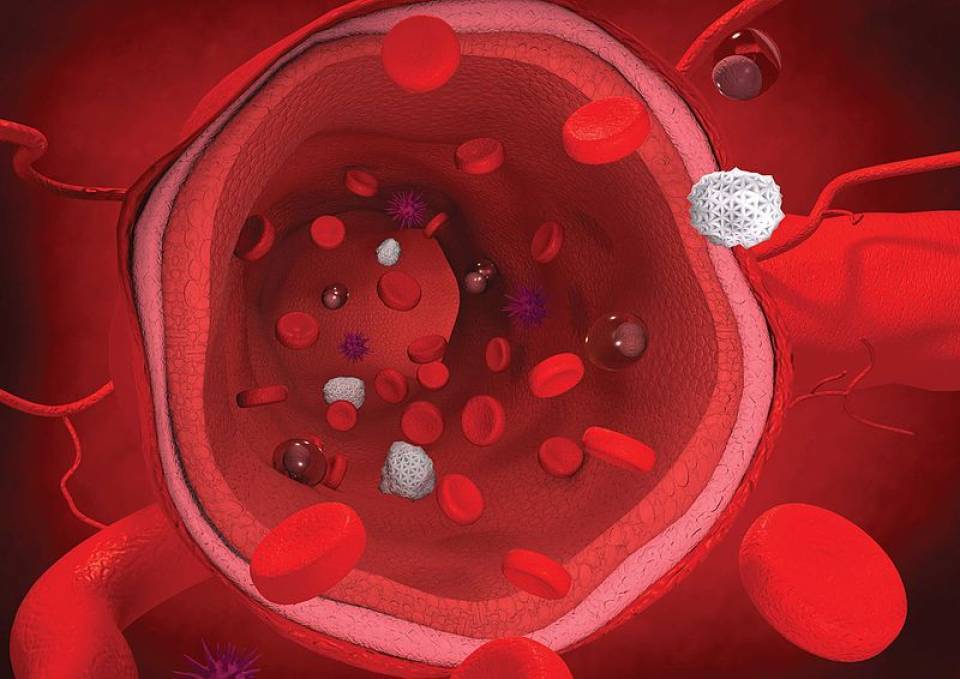
Familial hypercholesterolaemia is a hereditary disease characterised by an increase in low-density cholesterol levels in the blood, known as LDL-C. These patients have a greater risk of cardiovascular diseases such as heart attack.
Many people affected by familial hypercholesterolaemia never manage to reduce their blood cholesterol levels to recommended levels, even when taking the maximum dosage of the most effective medicine currently available. At the moment, the most effective drugs are statins in combination with ezetimibe, which inhibit the absorption of blood cholesterol. This medication has various contraindications in terms of safety and tolerance. Furthermore, it cannot be administered to minors, one of the groups affected by familial hypercholesterolaemia.
One of the treatments used in these patients when conventional medicine doesn’t work is apheresis. This is an invasive procedure similar to dialysis, in which the excess LDL in the blood is physically extracted using a machine. The LDL-free blood is then returned to the patient’s bloodstream. This procedure is expensive, invasive (as it requires vascular access), and difficult to obtain in many countries.
Some studies have demonstrated that evocolumab, a monoclonal antibody, manages to reduce LDL levels in the blood, as well as preventing degradation of the LDL-R (cholesterol receptors) in these patients.
A clinical trial, in which Hospital Clínic participated, proved the long-term efficacy of evocolumab in 300 patients with severe familial hypercholesterolaemia. As well as having familial hypercholesterolaemia, the participants also had high LDL levels that did not respond to medication, or had had cardiovascular diseases as a result of their illness. Of these 300 participants, 14 were under 18 years old. This study, known as TAUSSIG, is the longest clinical trial carried out to date with evocolumab as cholesterol medication.
Follow-up was carried out with these patients, treated with subcutaneous evocolumab, for four years. The results in terms of safety were good, both for the adult and adolescent groups. None of the patients developed antibodies against the treatment. LDL levels reduced persistently, both at the start of the treatment (12 weeks), and at the end (216 weeks, that is, 4 years).
In patients with a partial absence of receptors (heterozygous), their LDL levels descended much more: 90 mg/dl on average, compared to initial levels of 192 mg/dl. In patients with a total absence of receptors (homozygous), the LDL reduced 75 mg/dl, compared to initial levels of 329 mg/dl. This involves a 54% and 20% reduction of LDL, respectively.
Furthermore, 26% of patients who used to regularly undergo apheresis treatments were able to stop due to this blood cholesterol reduction.
Another of the most relevant findings of this study is the efficacy and safety of this treatment in minors, as it had very good results in the 14 adolescents who participated. Thanks to this, a specific paediatric study will be carried out which will help to confirm the safety of this antibody in minors.
In conclusion, this study demonstrates that evocolumab reduces blood cholesterol and decreases the need for apheresis in patients with severe familial hypercholesterolaemia that does not respond to conventional treatments. Nevertheless, more studies that include a greater number of participants are needed, including a control group, as well as use of double-blind methodology, which ensures greater objectivity in the results.
What causes familial hypercholesterolaemia?
Familial hypercholesterolaemia is caused by a genetic alteration. This alteration causes the blood cholesterol levels to increase for different reasons. The main reason is the loss of function of the lipoprotein receptors (LDL-R). These receptors are in charge of eliminating blood cholesterol at the hepatic level.
Most patients inherit this genetic alteration from one of their parents (heterozygous), and as such, the other copy of the gene, which comes from a progenitor who does not have hypercholesterolaemia, will not be altered. Another group of patients has the alteration in both genes (homozygous), as both progenitors have transmitted the altered gene. Depending on their genetic heritage, the patients will have a partial absence of receptors (heterozygous), or even a total absence of receptors (homozygous). This lack of receptors drastically diminishes their capacity to eliminate cholesterol from the blood.
Source: Dr. Zambón, doctor from the Institute Clínic of Digestive and Metabolic Diseases