An article published in the journal Scientific Reports and led by Olga Tura-Ceide, a researcher in the IDIBAPS group Pathophysiologic mechanisms of respiratory diseases directed by Joan Albert Barberà, of the Respiratory Diseases CIBER, and from the Girona Biomedical Research Institute (IDIBGI), provides new information on metabolic changes in chronic thromboembolic pulmonary hypertension (CTEPH) and pulmonary arterial hypertension (PAH).
CTEPH and PAH are two rare and severe forms of pulmonary hypertension (PH). Although the origins are different, in both diseases, blood flow through the pulmonary arteries is compromised. Furthermore, patients with CTEPH may present vascular abnormalities similar to those observed in PAH.
The body uses two main metabolic pathways to produce energy. The first, oxidative phosphorylation, occurs inside the mitochondria, the cell structures responsible for producing energy. The second, glycolysis, consists of breaking down glucose to obtain energy and takes place outside the mitochondria.
Under normal conditions, oxidative phosphorylation generates most of the energy the body needs. In PAH, however, the endothelial cells in the blood vessels undergo metabolic changes and glycolysis becomes the predominant mechanisms of energy production. These metabolic imbalances contribute to the uncontrolled growth and proliferation of the endothelial cells, which results in narrowing of the pulmonary arteries.
Unlike PAH, the metabolic alterations that occur in the pulmonary endothelial cells in CTEPH are less well known. This led Tura-Ceide and her colleagues to study and compare the metabolic profile of these cells derived from the pulmonary arteries of patients with CTEPH and patients with PAH.
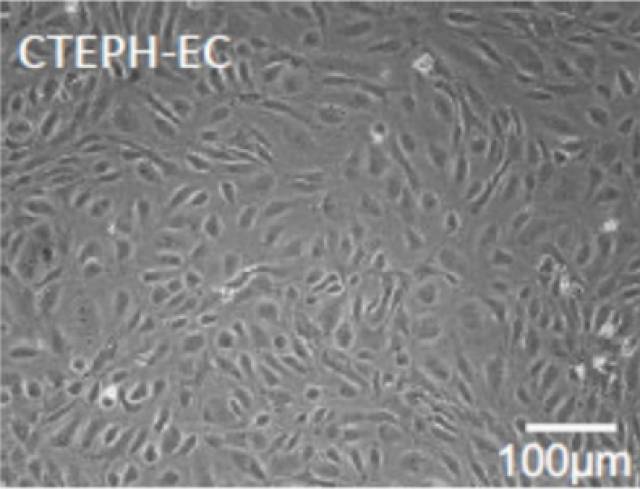
The results clearly show that both diseases differ with regard to the mechanisms of glycolysis, oxidative phosphorylation, and glutamine metabolism. Specifically, the endothelial cells of patients with CTEPH present a reduction in glycolysis and glutaminolysis, while the activity of these processes increases in PAH. These differences are important, as they provide information that makes it possible to design new, more specific, treatments for these diseases.
The study was financed with funds from the European Union (BIOTRACK-Marie Curie program), the Carlos III Institute of Health, the CIBERES Pulmonary Hypertension Line, and the Foundation Against Pulmonary Hypertension.
Article reference
V. F. E. D. Smolders, C. Rodríguez, I. Blanco, R. Szulcek, Wim Timens, L. Piccari, Y. Roger, X. Hu, Constanza Morén, C. Bonjoch, L. Sebastián, M. Castellà, J. Osorio, V. I. Peinado, Harm Jan Bogaard, P. H. A. Quax, M. Cascante, J. A. Barberà and O. Tura-Ceide. Metabolic profile in endothelial cells of chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension. Scientific Reports. 12, Article number: 2283 (2022) DOI:10.21203/rs.3.rs-1008061/v1