A team of researchers from the Clínic-IDIBAPS has evaluated the effectiveness of concentrated cognitive behavioural therapy (CCBT) to treat obsessive-compulsive disorder (OCD) in unmedicated children and adolescents.
Obsessive-compulsive disorder affects around 1% of children and adolescents and can be profoundly disabling. Traditional cognitive behavioural therapy, the standard treatment, often involves many sessions over several months, which sometimes makes it difficult for patients to follow. This new proposal seeks to offer a more agile and accessible solution. With CCBT, the participants experienced a significant reduction in OCD symptoms after an intensive one-month programme, and the benefits were sustained six months after treatment.
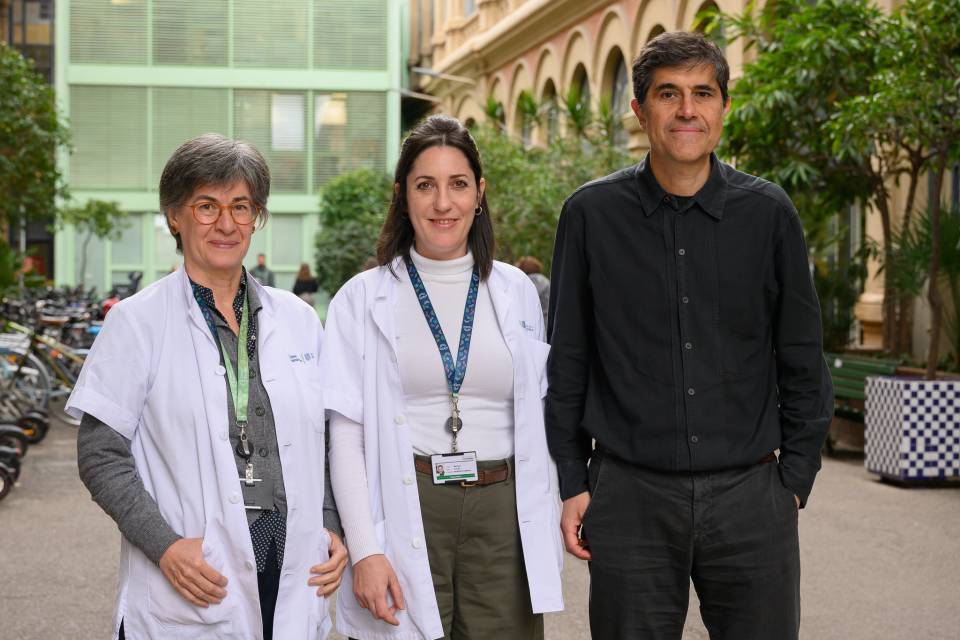
The research, published in the journal Behavior Therapy, was led by Dr Miquel A. Fullana, researcher in the IDIBAPS Imaging of Mood- and Anxiety-Related Disorders (IMARD) group and clinical psychologist in the Clínic Barcelona Psychiatry and Psychology Service, and Dr Luisa Lázaro, head of the Child and Adolescent Psychiatry and Psychology Service at the Clínic. Dr Laura Hermida, clinical psychologist in the Child and Adolescent Psychiatry and Psychology Service at the Clínic, participated as first author. In addition, researchers from other institutions participated in the study, both in Spain, such as the IDIBELL and the Sagrat Cor, and in Sweden, such as the Karolinska Institutet.
The study included 30 participants aged between 7 and 17 years old, who were not undergoing pharmacological treatment and who were randomly divided into two groups: one group received CCBT and the other was placed on the waiting list for treatment, as a control group. The CCBT consisted of a total of 20 hours, in 1.5-hour sessions spread out over a maximum of four weeks.
The results show that the participants who received the CCBT showed a significant improvement, with an average reduction in symptoms of 30% according to the CY-BOCS scale (used to measure OCD severity). Moreover, “the benefits were maintained in follow-ups at three and six months, which reinforces the durability of the treatment", said Dr Hermida. These improvements were observed when comparing the results with a group of patients on the waiting lists who did not receive any treatment. At the end of the study, the patients on the waiting list were offered CCBT, obtaining very similar results.
The study also observed that "the youngest children (7 to 12 years old) responded better to the treatment than adolescents, and that those with more severe initial symptoms had more room for improvement”, explained Dr Fullana.
Despite the limitations, such as the absence of a more robust control group and the small size of the sample, the researchers emphasise the potential of this approach to transform the treatment of OCD in paediatric populations. “This concentrated format not only facilitates access and reduces treatment time, it can also rapidly alleviate the burden of OCD in children, adolescents and their families”, concluded Dr Lázaro.
This breakthrough opens up new avenues for optimising healthcare resources and helping a greater number of patients, especially those living in areas with limited access to specialised services. The researchers hope that new studies with larger and more diverse samples will confirm and expand on these promising results.
Article reference:
L. Hermida-Barros, B. García-Delgar, S. Lera-Miguel, E. Forcadell, E. Moreno, M. Primé-Tous, N. Jaurrieta, X. Segú, E. Vilajosana, C. Soriano-Mas, L. Fernández de la Cruz, E. Vieta, J. Radua, L. Lázaro, M.A. Fullana, Concentrated Cognitive-Behavior Therapy for Unmedicated Children and Adolescents with Obsessive-Compulsive Disorder in Routine Clinical Care: A Randomized Controlled Trial with a 6-month Naturalistic Follow-up, Behavior Therapy (2025), doi: https://doi.org/10.1016/j.beth.2025.01.001