- What is it?
- Team and structure
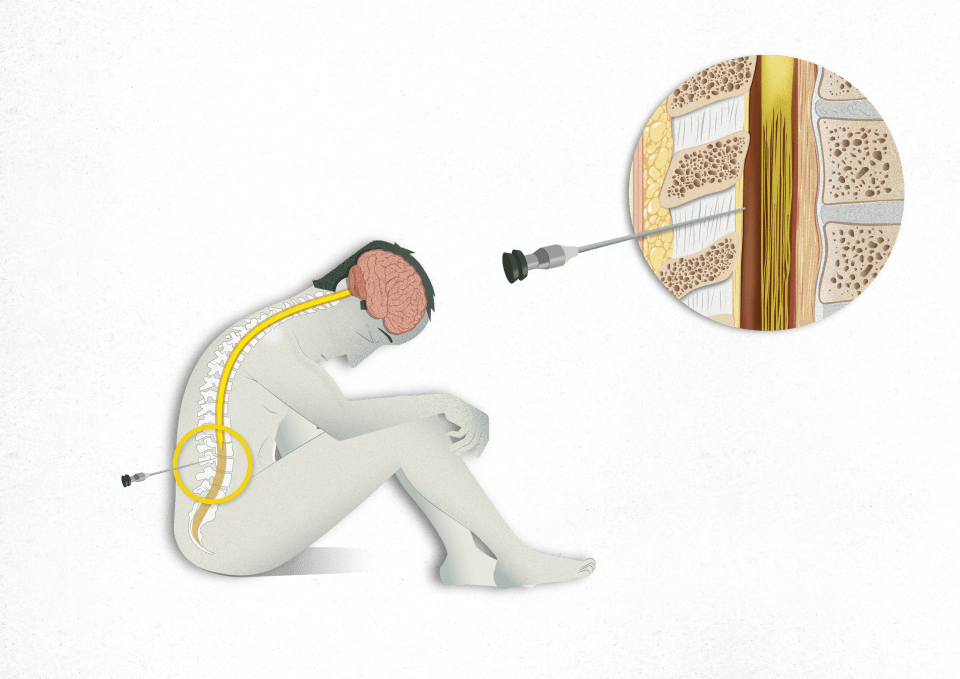
What is a Lumbar Puncture?
A lumbar puncture is a procedure used to diagnose different medical conditions. It is performed by inserting a needle between two vertebrae in the lumbar region, specifically where there is no spinal cord to prevent the risk of possible spinal cord injuries. It is done to extract samples of cerebrospinal fluid.
Cerebrospinal fluid (CSF) is a clear, transparent, water-like fluid found in the subarachnoid space, which is the space between the brain and the spinal cord and the membranes that surround them (the meninges). This fluid bathes the brain and spinal cord and its analysis provides valuable information about the health of the central nervous system and helps diagnose various diseases and medical conditions.
This test also allows other assessments to be made, such as measuring the pressure of this fluid or even administering medications.
When is this test necessary and what diseases can it diagnose?
This test is performed based on the clinical evaluation of healthcare professionals and their need to obtain additional information for the diagnosis and proper management of the patient. This test is indicated for:
- Detecting the presence of infectious agents such as bacteria, viruses or fungi in the cerebrospinal fluid which are indicators of infections in the central nervous system, such as meningitis and encephalitis.
- Diagnosing neurological diseases such as Alzheimer's disease, dementia with Lewy bodies or prion diseases, multiple sclerosis, autoimmune encephalitis, neuropathies and radiculopathy (trapped nerves), such as Guillain-Barré syndrome, as well as movement disorders.
- Detecting tumour cells in the nervous system, as occurs in some leukaemias and, less often, for tumours at advanced stages.
- Detecting the abnormal presence of blood in the cerebrospinal fluid (haemorrhage in the subarachnoid space) not observed in imaging tests.
- Measuring cerebrospinal fluid pressure (e.g., with intracranial hypertension).
In addition to being a diagnostic procedure, lumbar punctures can also be used therapeutically to administer medications directly into the subarachnoid space, such as anaesthetics, chemotherapy agents or drugs to treat specific neurological disorders. It can also be used to inject radiological contrast prior to an imaging test.
How should I prepare for the procedure?
In general, the test requires no specific preparation by the patient, but does require a series of rules to be followed:

If the test is essential for people who take an anticoagulant or two antiplatelet drugs, they must stop taking this medication in the days before the test, in accordance with the health professional’s instructions, to prevent the risk of serious bleeding.

It may also be necessary to do some tests to ensure there are no contraindications and to minimise the risk of complications. This is how an analysis is performed to check the patient has no coagulation problems and to minimise the risk of bleeding. A brain imaging test must also be performed to rule out the presence of any lesion at the intracranial level.

After performing the puncture, it is recommended to follow certain relative rest measures and hydrate abundantly during the following 24 hours to prevent the appearance of complications.
How is it performed?
- Positioning the patient. The position depends on the procedure to be performed: lying on one side in a foetal position with the head flexed or sitting leaning forward with the chin resting on the chest. These positions are intended to help open the spaces between the vertebrae where the needle is inserted. Patients have to remain as still as possible during the procedure to prevent difficulties or complications.
- Preparing the environment: Sterilisation and disinfection of the skin insertion area to minimise the risk of infection.
- Anaesthetising the insertion area to minimise discomfort using a cold spray or infiltrating with a subcutaneous needle.
- Lumbar puncture. This is performed with a long, thin needle called a spinal or Tuohy needle to penetrate the skin and tissues until it reaches the subarachnoid space. The needle is inserted between two lumbar vertebrae, usually between either the third and fourth or the fourth and fifth, depending on the patient's anatomy. Sometimes, more than one puncture is required to access the space, for example, in certain patients with back problems.
- A small amount of cerebrospinal fluid is collected in sterile test tubes for later analysis in the laboratory. This sample can be obtained by letting out the fluid dropwise or by removing it little by little with a syringe.
- The needle is then carefully withdrawn and a sterile dressing applied to the puncture site to help prevent infection.
Once the procedure is complete, patients must rest and ensure they are well hydrated. An observation period may be required to check for signs of complications, depending on the procedure performed.
Where is the test performed?
The location of the test depends on the patient's situation:
- When scheduled at the day hospital where the patient usually goes, the test is performed there, with the patient leaving once it is finished.
- If the person consults the emergency services, a test can be performed in the emergency booth, if the person is able to cooperate, or in the operating room if the patient requires sedation.
- If the test is indicated for a person already hospitalised, it is performed in the hospital bed.
Who performs the test?
The test is conducted by a specialist, with support staff providing the necessary instruments to carry out the procedure and collect the samples.
How long does the test last?
The test time depends on several factors, such as the anatomical difficulty of inserting the needle, the experience of the healthcare professional, the number of samples required and if any treatment has to be administered. However, it usually takes about 10-20 minutes. After the procedure, a period of rest and observation is usually required before the patient is allowed to go home; this is usually 20-60 minutes for a standard procedure.
What will I feel during the test?
Sensations felt during the test depend on whether or not anaesthesia is administered. If cutaneous anaesthesia is used, a very cold sensation is felt on the back. If subcutaneous anaesthesia is administered, a slight sting and itching will be felt when the drug is injected. If no anaesthesia is administered, the back will sting temporarily, similar to when having a blood test. Slight pressure or discomfort may be felt when the needle is inserted. Occasionally, an electric shock may be felt in one leg when the needle enters the subarachnoid space.
What are possible complications?
Complications depend on several factors, such as the patient's underlying health conditions, the technique used, the type of needle and adherence to aseptic and antiseptic measures. In general, when the lumbar puncture is performed in an appropriate environment with the proper measures, complications are rare and most patients experience none.
The most common complication that may occur is:

The appearance of a headache 24-48 hours after the procedure, known as a post-puncture headache. This appears in 5-40% of cases depending on the needle used and the difficulties in performing the test; it is more frequent in younger patients and those with a history of headaches. It is an oppressive headache at the level of the neck and head that appears when standing up and improves when lying down; it may be accompanied by nausea, vomiting, stiffness in the neck, blurred vision or tinnitus. It is usually controlled with mild analgesics, such as paracetamol or NSAIDs, and usually resolves within 24-48 hours; although sometimes it can last for up to 10 days or require specific treatment.
Other less common complications include:

Infection at the puncture site, either cutaneously or, more rarely, at the meningeal level (meningitis or epidural abscess). This risk is extremely low, especially if proper aseptic and antiseptic practices are followed during the procedure.

Local bleeding may occur at the puncture site in the form of a small bruise that disappears in the following days without further complications. In even rarer cases, bleeding may occur at the level of the spinal canal or intracranially in the form of a subdural or epidural haematoma. This manifests itself with pain and neurological disorders, such as motor or sensory deficits and incontinence. The risk of this complication is also extremely low if the patient has no coagulation disorders or takes anticoagulants.

There is a low risk of injury to nearby nerve roots during lumbar puncture, which may result in a root injury similar to a pinch. If the fluid study requires a large sample volume to be extracted, double vision or temporary hearing loss may appear due to a decrease in fluid pressure and involvement of the cranial nerves, which recovers as the fluid regenerates.
If, after having a lumbar puncture, you have a fever, feel weak in any part of the body, experience a loss of feeling, incontinence, a severe headache that is not controlled by the aforementioned measures or an altered level of consciousness, you should consult the emergency department.
Related contents
Substantiated information by:


Published: 27 August 2024
Updated: 27 August 2024
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox