Usually, each type of cancer is studied individually. In this case, multiple types of cancer that share the overexpression of this biomarker will be analysed, to see whether immunotherapy works irrespective of the location of the tumour. Immunotherapy involves the boosting of the body’s own immune system in order to fight cancer. Thus, this treatment does not target the tumour itself, but instead stimulates the body’s immune system. So, it is less toxic than standard treatments such as chemotherapy.
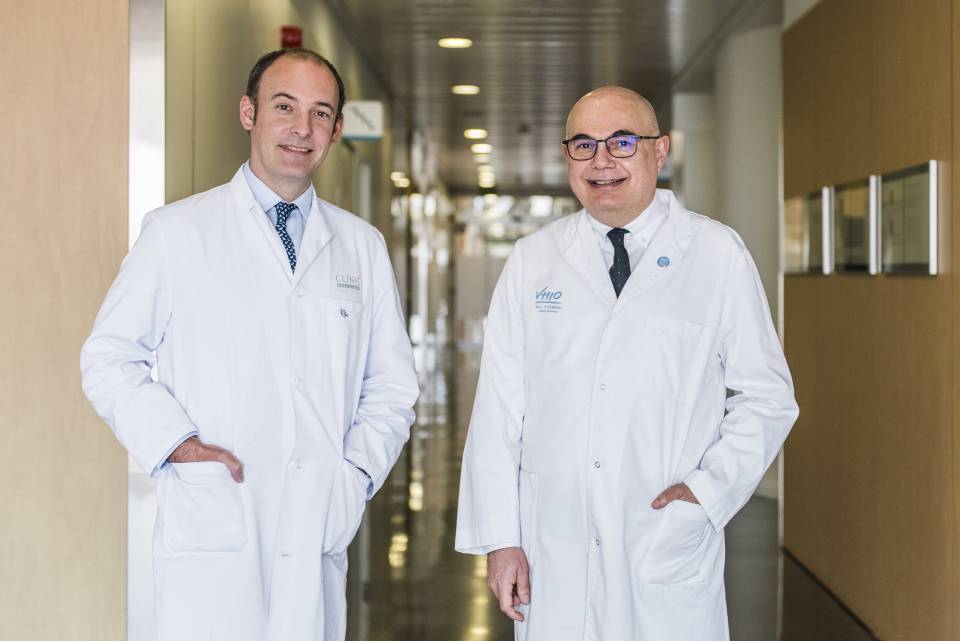
Dr. Aleix Prat, president of SOLTI, lead researcher at ACROPOLI, head of the Medical Oncology Service at the Hospital Clínic de Barcelona and head of the IDIBAPS Translational genomics and targeted therapies in solid tumours research group, points out: “This trial will allow for the participation of patients with less common tumours, for which less clinical research has been carried out and not as many treatments have been approved. In this case, we shall study whether, by using a specific biomarker, a subgroup of these patients can benefit from immunotherapy, as occurs in other more common types of cancer.”
Meanwhile, Dr. Josep Tabernero, director of the VHIO, co-lead researcher at ACROPOLI and head of the Medical Oncology Service at the Hospital Universitari Vall d'Hebron, adds: "One of our objectives of this basket trial is to show that the marker based on the PD-1 gene –using prior detection with messenger RNA– is more sensitive for determining the population of patients who can benefit from the treatment than the expression of the protein PD-L1 detected by immunohistochemistry, which is what we have been using up to now.”
Thus, the importance of the trial hinges on three main points: the identification of the patients for whom an emerging field such as immunotherapy can make a major impact; carrying this out using precision oncology, in other words via biomarkers that determine a priori which patients can benefit from this; and, finally, transversality, moving towards a type of study in which the location of the tumour is not the main objective.
Immunotherapy is a therapeutic strategy that has been in development for years, and the evidence indicates that it is essential to know the immune activation status of the patients’ tumours in order to predict whether the response to this type of therapy will be significant or not. It is a comparison of what are known as “cold tumours” –with a low quantification of PD-1 expression– with “hot tumours”, in which we find higher levels of PD-1.
Led by Dr. Aleix Prat and Dr. Josep Tabernero, in addition to the Hospital Clínic and the Hospital Universitari Vall d’Hebron in Barcelona, eight more hospitals are to take part in the trial, making a total of ten: the Fundació Institut Valencià d'Oncologia, the Hospital Clínic Universitari de València, the Hospital Universitari Sant Joan de Reus de Tarragona, the Hospital Universitario Fundación Jiménez Díaz in Madrid, the Hospital Universitario 12 de Octubre in Madrid, the Hospital Universitari Germans Trias i Pujol in Badalona (Barcelona), and the Institut Oncològic Barcelona (IOB) of the Hospital Quirónsalud Barcelona.
The aim of the ACROPOLI trial, which will last for two years, is to predict the benefits of treatment with the PD-1 inhibitor: spartalizumab. In the patients taking part in this trial, the PD-1 expression in their tumour will be quantified and they will be divided into two groups: one with a high expression, and another containing patients with a low expression, in order to demonstrate in which cases immunotherapy does not work