- What is it?
- Causes and risk factors
- Symptoms
- Diagnosis
- Treatment
- Evolution of the disease
- Living with the disease
- Research
- Frequently asked questions
- Team and structure
Frequently asked questions about Hypercholesterolaemia
Total cholesterol of less than 200 mg/dL is often put forward as an ideal level. While it is true that it may correspond to an ideal level to prevent cardiovascular diseases, it is not always the target value for all individuals, and just because you have a total cholesterol level of greater than 200 mg/dL it does not necessarily mean you require drug therapy.
Appropriate cholesterol levels for each person depend on several factors, in particular their cardiovascular risk factors, their age and the presence of cardiovascular diseases or other chronic diseases. Taking all these factors into account, it is advisable to discuss the matter with your healthcare team to discover your appropriate cholesterol levels.
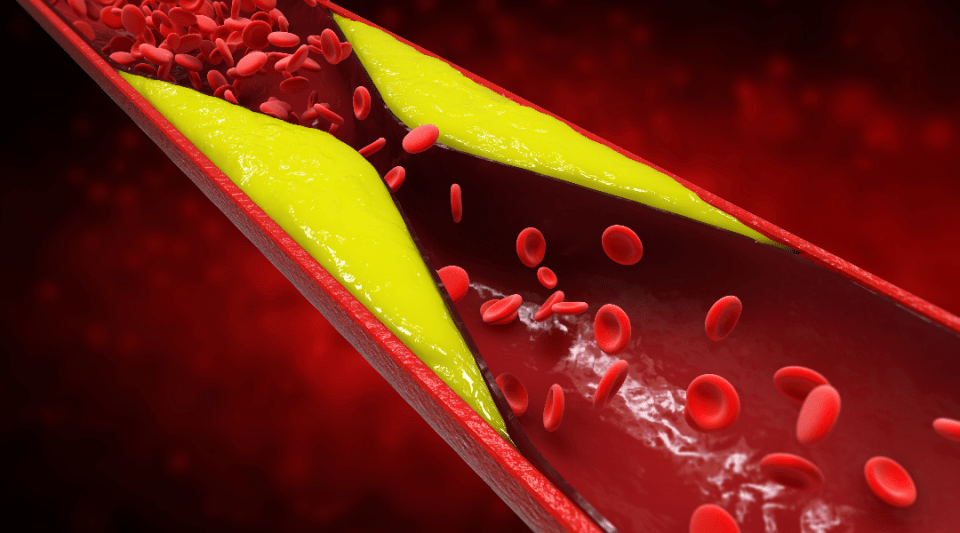
Cholesterol does not circulate freely in the blood. As it is a fat it cannot circulate in an aqueous medium, just like oil does not mix with water. However, it can circulate in the blood when it is packed inside small spheres called lipoproteins. These lipoproteins travel from the liver to the rest of the body (the tissues), and vice versa, supplying and extracting cholesterol. When cholesterol is supplied to tissues, it circulates inside LDL (low-density lipoproteins). Cholesterol circulating in LDLs is known as bad cholesterol because if the level is too high it forms deposits inside the arteries. The type known as good cholesterol circulates inside HDL (high-density lipoproteins) which transport the cholesterol from tissues (like the arteries) to the liver where it is released. Therefore, when HDL or good cholesterol is high, the arteries accumulate less cholesterol.
Patients with familial hypercholesterolaemia characteristically have high cholesterol levels that are very close to or above 300 mg/dL in adults, and/or they (or their close relatives, i.e., parents or siblings) have suffered coronary artery disease (heart attack or angina) before the age of 55 years in men or 60–65 in women.
It is a genetic disorder that causes high cholesterol levels from birth. You should ask your healthcare team if you believe you have familial hypercholesterolaemia, the suspected diagnosis is straightforward. If familial hypercholesterolaemia is confirmed or suspected, besides requiring drug treatment to reduce your cholesterol levels, your entire family should be studied. Most people who have this condition are unaware of it.
Triglycerides and cholesterol are two different types of fat. The fats we eat are mainly absorbed in the form of triglycerides that travel from the intestine to the liver where they are “packaged” and resent to the rest of the body as a source of energy to be stored in the fatty tissue. Cholesterol and triglycerides circulate in the blood packed inside small spheres called lipoproteins, which are comprised of different proportions of triglycerides and cholesterol. These “mixed” lipoproteins released from the liver are harmful if their levels are too high. When lipoproteins are formed almost exclusively by triglycerides, and their concentration is very high, they can cause inflammation of the pancreas (pancreatitis), and when they also contain cholesterol, they contribute to the development of atheromatous plaques. Therefore, although they are not the same, cholesterol and triglycerides are often associated with each other.
Familial combined hyperlipidaemia is a mixed hyperlipidaemia (or hypercholesterolaemia) – high cholesterol and triglyceride levels at the same time – that affects multiple members of a family and (when poorly controlled) is associated with premature cardiovascular problems in patients and/or their close relatives. Although it is a genetic condition, both cholesterol and triglyceride levels worsen considerably in patients with an unsuitable lifestyle (weight gain, inappropriate diet, lack of physical activity, etc.) and therefore lifestyle improvements and medication are considered essential to achieve correct control of the disease.
Pregnancy is a clinical situation in which cholesterol increases above usual levels. Do not worry, this is typical, and levels will return to normal after the delivery. Systematic measurement of cholesterol levels is not recommended in pregnant women. Pregnant women should follow the usual dietary recommendations and try to maintain a healthy heart, just as they should when they are not pregnant.
Medications for cholesterol are not recommended during pregnancy, so you should stop taking them if you are pregnant. If you are taking drugs for high cholesterol, you are advised to take precautions to avoid becoming pregnant. If you are planning to get pregnant, it is recommendable to discontinue cholesterol medication 2–3 months before trying.
For some women, contraceptives can induce an increase in cholesterol levels, which is occasionally quite significant. If the level is still not under reasonable control after improving your diet, you should consider changing the contraceptive method or evaluating treatment for high cholesterol based on your family medical history and risk factors.
The first thing is to find out why your child’s cholesterol levels are too high. Your paediatrician will provide an explanation. In children, as with adults, there has been an increase in overweight, unhealthy dietary habits and a sedentary lifestyle. These factors can cause high cholesterol and triglycerides. On the other hand, children with familial hypercholesterolaemia must also be identified during childhood and parents and siblings should be evaluated whenever the disease is suspected. If the condition is confirmed, children should start drug treatment aged between 8 and 14 years on a case-by-case basis. Drug treatment is also safe in children of this age range.
No medicine is free from potential side effects. However, when discussing drugs regulated and approved by official medicines agencies, the benefits they give to people who need them are considered to far outweigh any potential harm or side effects, which are rare, mild or temporary.
Statins are safe drugs; we have a lot of experience with them, they are well known and have proven to be of great benefit in the reduction of cardiovascular diseases. In some people, less than 5%–10% according to studies that have evaluated them in detail, they can cause muscle aches, above all at the start of treatment, which disappear when the dose is reduced or if a different statin is used. In any event, the muscle aches are neither persistent nor permanent once the medication is discontinued.
Traditionally it was said that statins should be taken at night because it increases their effectiveness. Nevertheless, what really matters is to take them every day; so if taking them in the evenings means you are more likely to forget them, you should select the most convenient time for you to ensure you do not miss any.
While a small percentage of patients can experience muscle aches with statins, most patients who take them do not present any symptoms, so they can practice sport as usual, including at a competitive level.
The most reliable, exhaustive, and independent scientific evidence collected over more than 30 years has shown that high cholesterol levels increase the risk of a heart attack or stroke. The same can be said about cholesterol-lowering drugs (above all statins) and the reduced risk of suffering a cardiovascular problem. In fact, in light of these false reports many national and international scientific societies have decided to protest through official letters of complaint. You should never stop taking cholesterol-lowering drugs because of alarmist headlines without first verifying their truthfulness with your healthcare team.
Statins cause a very small increase in blood sugar levels which only occurs in a very small percentage of people who take them and in any case this side effect is overwhelmingly eclipsed by the benefits in terms of a reduced risk of a heart attack or stroke. Given that people with diabetes have a greater risk of suffering a cardiovascular event than people who do not have diabetes, then statins are especially indicated in this group of patients.
These are natural foods that contain a component other than just their nutritional value and which can help reduce cholesterol levels. They can be prepared by removing a component from the food (e.g., skimmed milk), by adding one (milk with vegetable sterols or phytosterols) or by replacing one (e.g., replacing the fat in milk with vegetable fat). Soluble fibre enriched foods (at a daily dose of at least 3 g/day) can also decrease dietary cholesterol absorption.
Among the simplest and most natural cholesterol-lowering “functional” foods that do not require any processing are nuts, pulses, whole grain cereals and dark chocolate.
Nutraceuticals are concentrated dietary supplements (in capsule, tablet or powder form) of one or more natural substances which, at doses greater than those found in foods in their natural form, can have a favourable effect on, for example, cholesterol levels. Red rice fermented by a specific yeast contains an active substance called monacolin K which is chemically very similar to lovastatin, a drug used to reduce cholesterol. Concentrated red yeast rice, alone or in combination (e.g., with coenzyme Q10, polyphenols, omega-3 fatty acids, berberine, policosanol and other substances), is available as a cholesterol-lowering product with a moderate effect (producing a reduction of up to 20%–30%). Its long-term beneficial or harmful effects are unknown, and it is not without side effects.
Phytosterols are vegetable compounds that are chemically similar to cholesterol. They are found naturally in certain foods such as vegetable oils, vegetables, dried fruits, nuts, cereals and pulses. Thanks to their structural similarity they compete with cholesterol during intestinal absorption, so more cholesterol remains unabsorbed in the gut and is eliminated in faeces, thus reducing its concentration in blood.
Used as a functional food, in other words, in preparations containing 2–3 g of different phytosterols or in supplemented foods (e.g., margarines), and taken during or after meals, they can contribute to a moderate reduction in total and LDL cholesterol of 7%–10%. This effect is additive when taken in combination with lipid-lowering drugs.
The red yeast fermented on the rice naturally produces a statin (lovastatin) and therefore it must not be taken along with conventional statins. Although these compounds can be bought over the counter in pharmacies or herbal stores, you should talk with your medical team before you start taking them. Foods enriched with vegetable sterols (in Spain they are available in most supermarkets, primarily as small-format dairy products) can generally be consumed at the same time as cholesterol-lowering drugs.
Omega-3 capsules (mainly composed of fish oil) can be found in a range of shops such as health food stores and pharmacies. They largely reduce triglycerides (at high doses of 2–4 g/day), with very little effect on cholesterol, so they must never be used to substitute drugs which genuinely lower cholesterol levels, that is, statins or ezetimibe. Nor have they proven to be effective at reducing the risk of cardiovascular problems.
Typically, they should use cooking methods that require very little fat such as grilling, boiling, steaming, roasting or using a griddle, reserving fried and stewed foods for special occasions. You should use vegetable oil when frying (olive oil is the best option) and do not reuse the oil.
There are no forbidden foods, but you must limit your consumption of saturated fats in your daily diet. Saturated fat is found in full-fat dairy products, butter, cream, red meat, cured meats, pastries and processed foods, amongst others.
Drinking alcohol is not a healthy habit, healthcare staff should not recommend it. If you decide to drink alcohol, you should only drink moderately (e.g., no more than one glass of wine per day) and avoid drinks with a high alcohol content. Alcoholic beverages have a high calorie content (alcohol and sugars) and their consumption can lead to overweight and obesity. Heavy consumption increases triglyceride levels.
- Cholesterol is only a matter of numbers. Cholesterol causes cardiovascular diseases, but a simple, isolated cholesterol value provides very little information, the doctor must assess the overall cardiovascular risk in patients with high cholesterol levels.
- Arteriosclerosis only affects elderly people. At present, a high percentage of the population have one or more cardiovascular risk factors that favour the onset of arteriosclerosis at an earlier age (40–50 years) than typically observed in the past.
- Women are better protected against cardiovascular diseases associated with high cholesterol. In Spain, cardiovascular disease is responsible for 24.6% of deaths in men and 22.5% in women. Cardiovascular care, including the evaluation and, if necessary, treatment of cholesterol levels, must be assessed from an early age in both men and women alike.
- It is unsafe to reduce cholesterol levels to very low values as it goes against cardiovascular safety. Attaining very low levels of bad or LDL cholesterol through drug treatment, especially in patients who have suffered a cardiovascular event (heart attack, stroke or lower extremity arterial disease), does not have any adverse effects and can reduce the risk of another cardiovascular problem.
- The Mediterranean diet is limited to olive oil and fish, it is expensive, impossible to follow and does not reduce the risk of arteriosclerosis. It is important to know that the Mediterranean diet is based on eating a wide variety, not just a small group, and mixture of products: mainly whole grain cereals, pulses, fruits, vegetables, nuts, small amounts of meat and dairy products, in addition to olive oil and fish. The Mediterranean diet prevents cardiovascular diseases. This prevention diet must also be accompanied by other healthy heart lifestyle habits such as regular physical exercise suitably adjusted to each person’s condition.
Substantiated information by:






Published: 2 October 2018
Updated: 21 October 2025
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox