- What is it?
- Symptoms
- Causes
- Tests and diagnosis
- Treatment
- Disease evolution
- Living with disease
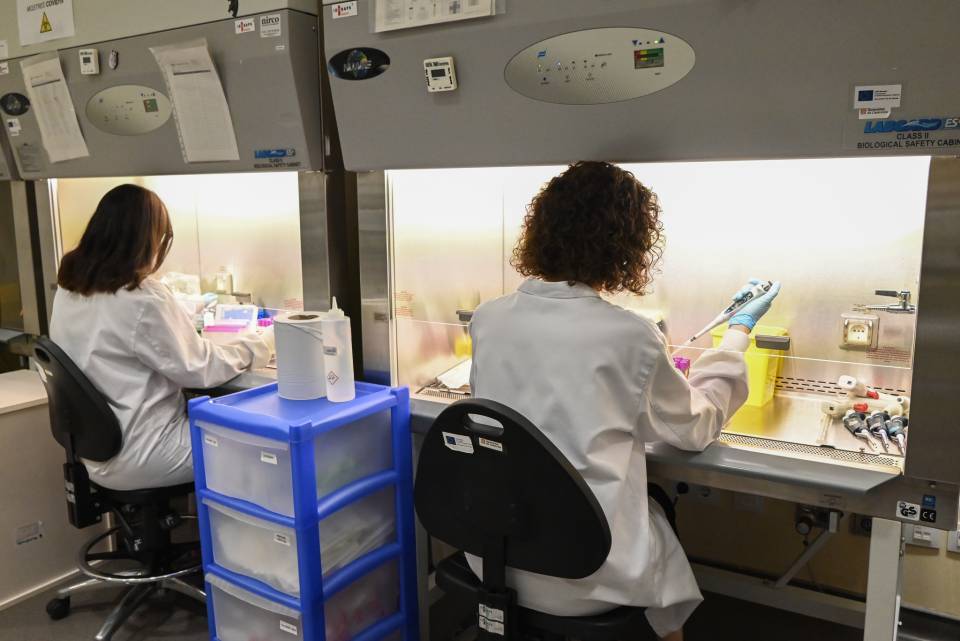
- Research lines
- Frequently Asked Questions
- Prevention
Frequently Asked Questions about Chronic Obstructive Pulmonary Disease
What’s wrong with me?
The most common symptoms of COPD are shortness of breath (dyspnoea), abnormal sputum and a chronic cough. It is a disease that gets worse with time, and for those who suffer from it, daily activities like climbing stairs can be difficult.
COPD is a chronic disease that is incurable, but can be controlled if the treatment is followed correctly. Depending on the severity of the disease, there may be periods when the symptoms are more severe, and it is recommended to be under the control of a chest diseases specialist to receive education about your disease.
The feeling of shortness of breath does not mean you need oxygen. It is only indicated if the level of oxygen in the blood gas analysis is low.
The first step is to eliminate the exposure to tobacco smoke. Patients who quit smoking have less symptoms and experience a slight improvement in lung function. Always follow the treatment prescribed by the health staff that attend you.
The signs that the disease is getting worse are the increase in shortness of breath, cough, changes in the appearance and quantity of sputum, fever, drowsiness and/or headache, swelling of the feet (oedema), an increase in the need of bronchodilator medication (rescue spray), and poor tolerance to usual activities.
In these cases, check that you have not forgotten to take the treatment. Remember that poor control of the "other diseases" that you may suffer from can contribute to the decompensation of your lung disease. Try to relax, anxiety episodes do not help COPD. Anxiety (fear, distress) can increase the usual symptoms. Depression (sadness, apathy, fatigue) make it difficult to assess the changes. Review the recommended "action plan".
What tests will I undergo?
The presence of COPD is confirmed by a simple diagnostic test, called spirometry, which measures the amount and velocity of inspired and expired air. Despite this, it is an under-diagnosed disease. As COPD is a disease that progresses slowly, it is generally diagnosed in people over 40 years old.
Spirometry is a non-invasive test that helps to measure the lung function of a person. It consists of breathing through the mouth into a small tube and forcing the breathing in order to measure the air flow.
As well as spirometry, there are other tests that can be useful. These include a chest x-ray, which shows if you could have emphysema, as well as rule out other lung problems or heart failure; laboratory blood tests (full blood count) to exclude other conditions at the time of the diagnosis; computerised tomography (CT scan) of the lung, also to determine if there is emphysema and to find out if the patient my benefit from surgery, as well as to warn of lung cancer; and an arterial blood gas analysis, which measures how the blood transports oxygen and removes carbon dioxide.
What treatments are available?
The lungs do not regenerate in COPD. However, with specialist medical treatment and specific exercises the efficiency of the rest of the lungs can be improved.
Nowadays, all Primary Health Care Centres and the professionals that work in them are prepared to help you and advise you on the best option. Therefore, the first thing is to consult with your family doctor and listen to his/her advice.
If the medication is prescribed only once per day, you should take the forgotten dose as soon as you remembered it. If this is not the case, continue with the established prescription. Under no circumstance should you double the next dose if you have forgotten to take the previous one.
All medications have side effects, but the benefits are better. Not everyone experiences side effects. If you have any doubts or have a new symptom, it is advised that you get in touch with the team that attends you.
If your medical team has prescribed oxygen it is because they have assessed that you need it at a particular time, but it may not be for the rest of your life. In the clinic they will carry out an assessment and follow-up of the oxygen therapy and the need on whether or not to continue with the treatment will be assessed.
For people with COPD, breathing rehabilitation is a very important part within the integral treatment of your COPD. If you are take part in the breathing rehabilitation program, your exercise capacity, your physical functioning, and your quality of life will improve.
Living with COPD
No. A single cigarette is bad for your COPD and any other type of smoking-derived diseases.
A correct diet leads to a better quality of life. It is recommended that meals are light, not very big, and several times a day. Avoid foods that may be difficult to digest and cause flatulence and that are too cold or too hot. You must drink 1.5 litres of water a day.
It cannot always be avoided, but may be prevented by some simple pieces of advice, such as giving up smoking and avoiding indirect or passive smoking. It is the best way to slow down the lung damage. It is important to distance yourself from people with colds; wash your hands; have the recommended vaccination; avoid cold air and sudden changes in temperature, as well as contaminants in the air, such as chimney smoke and dust, outside the home; and follow a healthy lifestyle and keep active; follow a balanced diet, and drink liquids.
The flu virus can cause a worsening of your COPD. Each year, on there not being a contraindication, you should have the flu vaccine as the virus changes every year. Go to your Primary Care Health Centre which will tell you when the vaccination campaign begins, which is usually the beginning of autumn.
Dogs and cats make very good company, but they also fill the house with hairs or skin particles, which can irritate the lungs. If you have pets, you must keep them clean and with the hair well cared for and brushed, and at bedtime they have to be outside the bedroom.
You can continue to travel, taking into account that you have to plan it in advance. Ask for help and advise the team that attends you, and if you need oxygen get in touch with the company that supplies your equipment.
Substantiated information by:


Published: 20 February 2018
Updated: 20 February 2018
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox
Chronic Obstructive Pulmonary Disease (COPD) related news
8 August 2024
Climate Change and its impact on Public Health
3 November 2021