Treatment of Cephalalgia
Firstly, it must be known what type of headache the patient has. Secondly, if there are any triggers, such as a change in sleep pattern or the taking of any food or drug, they must be identified and controlled. Healthy life habits have to be promoted, like maintaining regular sleeping hours, exercising, avoiding tobacco and alcohol, a balanced diet and avoiding constipation. And thirdly, a prescription for the treatment of acute attacks of pain should be given.
For migraine it is very important to start the acute treatment as near as possible to the onset of the appearance of the headache. Non-steroidal anti-inflammatory drugs with a rapid gastric absorption or triptans are used.
For tension headaches the use of relaxation techniques is chosen, along with exercise, anxiolytics, or paracetamol. In hemicranial headache indomethacin is prescribed, and in cluster headaches, subcutaneous sumatriptan or intranasal zolmotriptan.
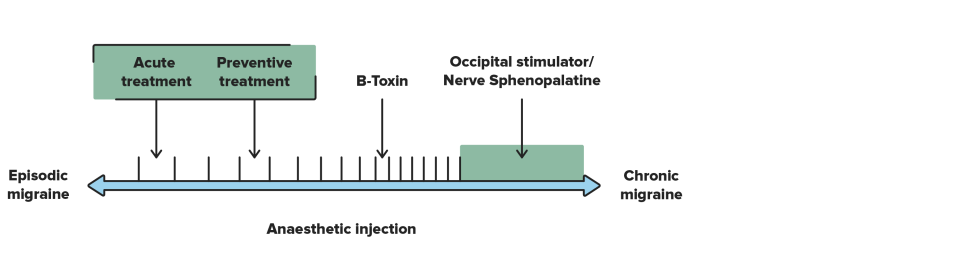
In any case, it must be taken into account if the patient, despite following the previous prescriptions, is a candidate to receive continuous or preventive prophylaxis treatment in order to reduce the number of episodes and their intensity and to prevent the headache from becoming chronic.
50% of patients with headache self-medicate, which often leads to the pain becoming chronic.
Treatment of Migraine
Managing a migraine attack
Migraines must be treated with a triptan as soon as the headache begins; that is, when the migraine is still mild. There are various types, doses and forms of the medication; the healthcare team will suggest the most suitable for the patient.
If there is no improvement within 2 hours, an anti-inflammatory drug is taken. If symptoms persist after another hour, a muscle relaxant and rest are advised.
Two newer drugs are available if triptans fail to provide relief:
- Lasmiditan (a ditan). The patient should not drive for 8 hours after administration due to potential adverse effects on the central nervous system, like dizziness, nausea and drowsiness. The drug is suitable for those with cardiovascular risks or a history of stroke or ischaemic heart disease (infarction).
- Rimegepant (a gepant). This drug is indicated as a preventive treatment for migraine. Its effectiveness in perimenstrual or menstrual migraine is being studied.
Overusing medications is one of the factors that can lead to chronic migraines, and so must be avoided. Overuse is considered as taking more than 15 anti-inflammatory drugs or 10 triptans per month.
Preventive treatment
In general, preventive treatment is indicated when:
- There are three or more migraine attacks a month.
- If a symptomatic treatment is being taken two or more days per week.
- If the attacks are severe with no adequate response to the treatment or with contra-indications or secondary effects to them.
- If the attacks are with a prolonged aura or with a severe neurological focus.
The choice of one or other drug does not only depend on its efficacy, since there are no large differences between them. It is chosen based on the patient’s profile, individualising the treatment depending on the possible secondary effects that they may cause; avoid increasing weight in females, impotence in males, making any depressive symptoms worse, etc.
As regards preventive treatment, in order to be effective, it has to last a minimum of between 3 and 6 months, and the optimum dose should be reached before rejecting it. There is a delay time between when it is started until it is effective that can vary between 10 days and 4 weeks. The treatment is considered effective when the frequency or intensity of the headache days is reduced by 50%. Once it is decided to withdraw it, it must be done slowly and gradually (1 month) and, in cases of refractory migraine, the doctor may recommend combining drugs.
The treatment is considered effective when the frequency or intensity of the headache days is reduced by 50%.
New treatments
In this section new treatments are described that, due to their complexity or elevated cost, are administered exclusively in specific Headache Units.
- Botulin Toxin. Currently it is only indicated in cephalalgia for the treatment of chronic migraine (patients that have more than 15 days of headache a month for the last three months, of which at least 8 fulfil migraine criteria). Even so, it has been effective in some patients with cluster headaches, trigeminal neuralgia, or nummular (coin-shaped) headaches.
The demonstration of its efficacy against a placebo in chronic migraine was obtained from two studies, PREEMPT I and PREEMPT II, which, between them, included more than 1,300 patients.
The treatment consists of injecting onabotulinum toxin A into different points of the pericranium musculature, blocking the peripheral sensitivity of the nociceptive receptors.
It is a straightforward technique in the hands of a trained neurologist, which does not affect the daily life of the patients, since they can continue their daily activities and with few secondary effects: pain and weakness in the neck, drooping of the eyelids, elevation of the eyebrow, discomfort at the injection sites.
In the long-term, according to the data of patients treated during more than 5 years, no new secondary effects have appeared, except two cases reporting an insignificant atrophy in the frontal and temporal muscles.
Half of the patients responded to the first session, 11% to the second, and 10% to the third. This is why it is recommended not to reject the treatment until has been tried on two occasions. On the other hand, the effect expires at three months; therefore, the treatment is repeated at this interval. It is possible that the response to the usual dose of 155 units is insufficient and it is decided to increase the dose to 195 units.
Understanding CGRP
CGRP is a protein that dilates blood vessels, among other functions. When the nervous system is activated by a migraine trigger, CGRP is released, leading to pain from irritated sensitive nerves and inflammation in the area. This results in symptoms such as severe headaches.
- Anti-CGRP monoclonal antibodies. These drugs are highly specific, directly blocking the activity of CGRP, and are thus effective. They are administered once or twice a month and have long-lasting effects. There are 4 drugs in this group: 3 subcutaneous (erenumab, galcanezumab, fremanezumab) and 1 intravenous (eptinezumab). The three subcutaneous drugs are self-injectable; i.e., can be administered by the patient. The intravenous drug is fast-acting, within 24 hours.
These drugs have proven highly effective in halving the number of headaches per month. They are also indicated for patients who have not responded to other oral preventive treatments and botulinum toxin, as well as those with high medication use.
The side effects of injectables include skin irritation, so it is recommended to take a photo of any reaction for the health team to review. They should be used with caution by patients with cardiovascular or digestive problems (such as constipation). - Gepants. These are another option for blocking CGRP, but are taken orally. They are useful for both treating migraine attacks when they occur and for preventing them. Some types (ubrogepant, rimegepant and zavegepant) are used as acute treatment for migraine, while others (atogepant and rimegepant) are used as preventive options.
In Spain, only atogepant is approved as a preventive treatment for episodic and chronic migraine, while rimegepant is used for acute and episodic preventive treatment.
Common side effects are mild, such as nausea or dizziness, and they have shown good results even in people who have not responded to other treatments.
- Nerve blocks. Anaesthetic blocks constitute a therapeutic resource for the management of various headaches, either alone or in combination with other treatments. Local anaesthetics act by reversibly inhibiting the production and conduction of the stimulus of any type of excitable membrane, especially in nervous tissue. In clinical practice, the most widely used technique is the greater occipital nerve (GON) block.
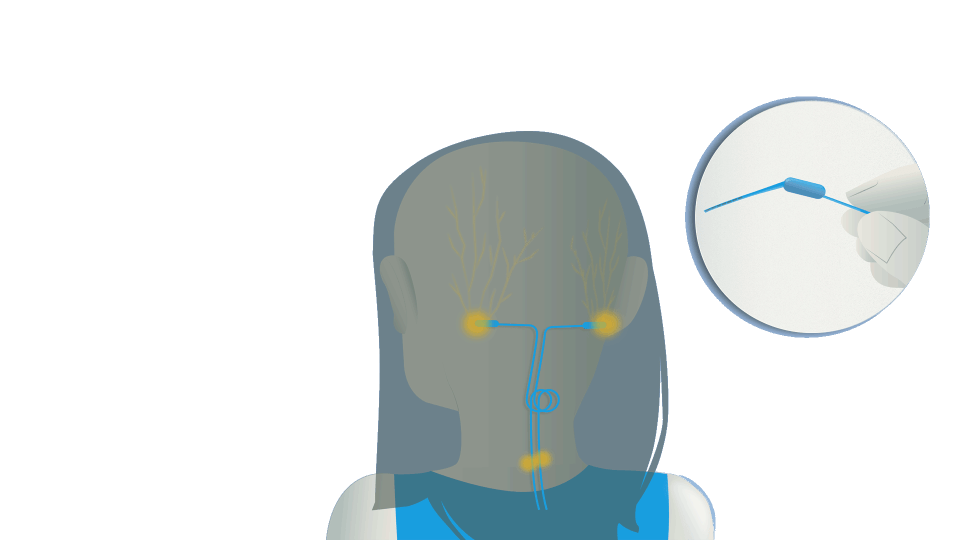
There is increasing scientific evidence supporting the modulatory role of the occipital nerves on the nociceptive afferents conveyed by the trigeminal nerve. By blocking the arrival of nociceptive impulses through the first cervical nerves, the anaesthetic block (AB) can act on this trigeminal-cervical complex, also inhibiting the transmission of trigeminal afferents.
They are used in migraine, trigeminal-autonomic headaches, cervicogenic headaches, post-traumatic headaches and in various neuralgias: occipital nerves (Arnold's neuralgia), supraorbital, supratrochlear, lacrimal, infratrochlear, infraorbital, external nasal and auriculotemporal nerves.
There is some heterogeneity in applying these techniques, which led to the Spanish Society of Neurology publishing the “Consensus Guide on Anaesthetic Infiltration Techniques for Pericranial Nerves” in 2016.
Other techniques are used to increase the precision of the block when it has been effective but of short duration, and pain is persistent: -
- Radiofrequency techniques. These consist of emitting small electromagnetic pulses to act on the peripheral nerve endings to reduce transmission of the pain. Its side effects include skin burns, pain and coagulation that, in general, improve over time.
- Sphenopalatine ganglion block. This is performed transnasally, using a specific device. The sphenopalatine ganglion is a small group of nerve cells at the back of the nose, and are the largest outside of the brain. It is connected to the trigeminal nerve that transmits sensations such as pain and temperature from the face to the brain. This ganglion has functions related to sensitivity and the response of the nervous system controlling calmness and stress.
The treatment can be performed outside the operating theatre without general anaesthesia.
- Non-invasive neurostimulators. There are 4 techniques approved by the US Food and Drug Administration. Cefaly, Vagus Nerve Stimulation, Transcranial Magnetic Stimulation and Sphenopalatine Ganglion Stimulation; although none is currently available in Spain. Their exact mechanism of action for controlling headaches is not known. They have demonstrated partial efficacy in the treatment of both acute and preventive pain, with good tolerance. They are designed to be applied by the patient themselves, and require a medical prescription.
- Invasive neurostimulators. There are basically two types: the greater occipital nerve and the sphenopalatine ganglion. Due to their related problems (electrode migration, need for surgical revisions, infections and intolerable paresthesia) they are indicated when there is no response to previous treatments and for particular situations.
- Deep brain stimulation. This consists of implanting the neurostimulator in the deep structures of the brain. Currently, successful operations have been performed on patients with refractory cluster headaches.
- Surgery. In this case, an operation is performed to decompress the contact between the nerve and an artery as a result of neuralgia, neurotomy or on a section of the affected nerve. An individual, specific and comprehensive study of each patient, including a proper risk-benefit analysis, must be performed by a multidisciplinary healthcare team before any appropriate technique is indicated.
Substantiated information by:


Published: 16 May 2018
Updated: 20 March 2025
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox