Thrombosis is a serious public health problem. Cardiovascular diseases accounted for 32% of deaths in the world in 2019, of which 85% were due to a heart attack or a stroke. A large number of these occur due to coagulation problems that result in a thrombosis. Coagulation disorders are also caused by a significant proportion of cancers. This increases the impact of thrombosis on the health of the world population.
Thrombosis is caused by an imbalance in blood coagulation mechanisms. Coagulation mechanisms provide vital functions for an organism, such as preventing excessive blood loss following a wound, among others. Current treatments for thrombosis affect coagulation mechanisms, and these have side effects. For this reason, research is continuing on new drugs to act on a thrombus without affecting the rest of the coagulation mechanism functions.
Why does thrombosis occur?
Thrombosis is a malfunction of haemostasis: the property of keeping blood (haemo-) in correct balance (-stasis); so that it circulates freely through arteries and veins. When a blood vessel ruptures, to prevent blood loss through it, haemostasis mechanisms are activated that form a clot to close the vessel and allow blood flow to be maintained. These clotting mechanisms are compensated by other anticoagulant mechanisms found in the blood. That is why we speak of a haemostatic balance between pro- and anticoagulant mechanisms.
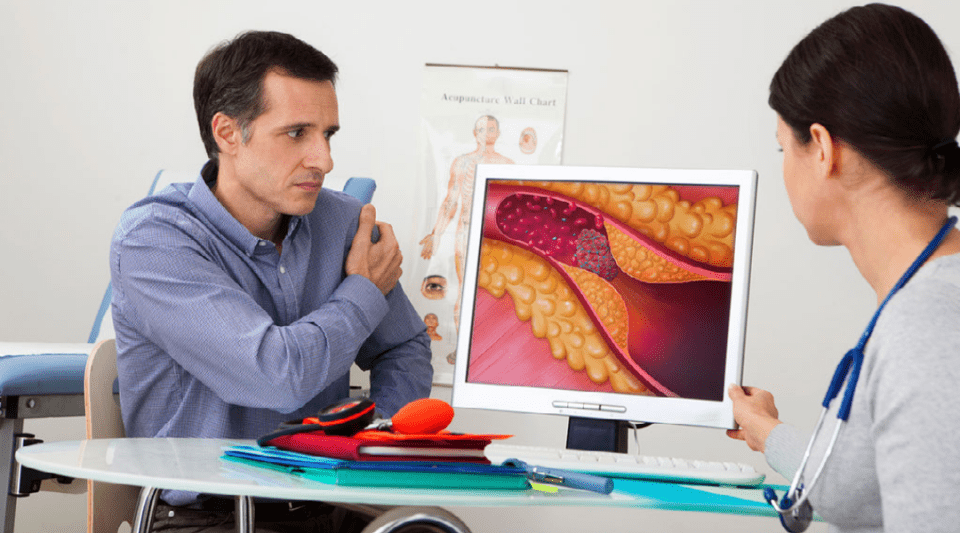
When there is damage to the inside of a vessel, either due to inflammation or fat accumulation (atherosclerosis), the haemostatic balance is affected and a clot forms within the vessel itself. This is known as a blood thrombus. If this clot moves through the bloodstream, it is called an embolism. A large proportion of deaths from heart attack, stroke and pulmonary embolism are the result of thrombosis in different organs.
How can thrombosis be treated?
Oral anticoagulants have contributed to reducing mortality in the population by reducing the risk of thrombosis. However, as this type of medication inhibits the body's ability to clot blood after an injury, one of its side effects is an increased risk of haemorrhaging (high blood loss).
Early oral anticoagulants had an effect on the coagulant action of vitamin K. In recent years, other direct-acting oral anticoagulants have been developed. These drugs specifically inhibit proteins essential for clotting or thrombus formation (thrombin and coagulation factor X). They are taken orally and do not require as much monitoring as classic oral anticoagulants, since their effects on patients are not so variable. In addition, in most clinical trials, they have been shown to be safer pharmacologically, due to not having as much risk of inducing bleeding.
Nevertheless, the search continues for new drugs that act specifically on thrombosis without affecting blood haemostasis and, therefore, maintaining its coagulation capacity in case of injury. This is a challenge, as there is increasing evidence that coagulation mechanisms are also involved in both the inflammatory response necessary to protect against infection and in tissue regeneration mechanisms.
AUTHOR:
Dr Pablo García de Frutos, Clínic-IDIBAPS Haemotherapy-Haemostasis Research Group.