One of the most important points that can be drawn from this study is the consequences of poor adherence or compliance with treatment. In the case of SLE, a lack of adherence has been associated with greater disease activity, that is, a greater risk of outbreaks. Outbreaks give way to greater accumulated damage in different organs (for example, in patients with kidney involvement, the possibility of losing kidney function and requiring dialysis) and, therefore, a worse quality of life. In the most severe cases it can even cause death.
What’s more, patients with SLE who do not adhere to treatment require more hospital admissions and treatments and visit the emergency services and day hospitals more often, among other problems. In short, non-adherence generates more complications, puts patients’ health at risk and unnecessarily increases health spending.
Two of the obstacles to identifying and correcting patients' habits is that they do not admit they are not properly taking their medication, or that they are not adequately following the guidelines prescribed by their health professionals. This occurs frequently and can confuse medical professionals, who might believe that the medication prescribed is not sufficient to control the disease; this in turn may lead them to either increase it or change it to something stronger, producing more side effects.
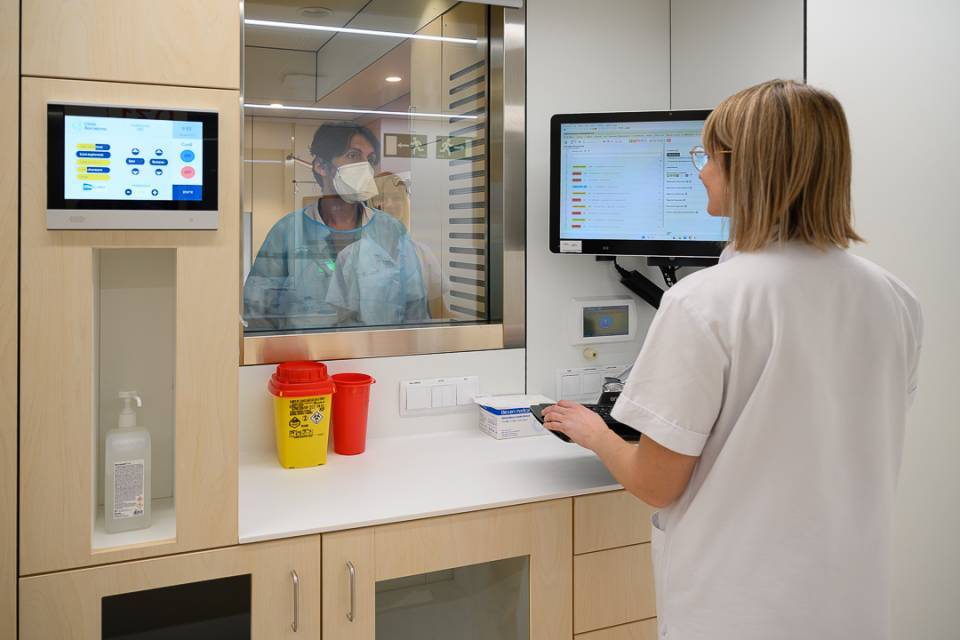
To put an end to these complications that hinder an adequate control of the disease, it has been observed that - despite the fact that it is the patient's responsibility to properly comply with prescribed treatments - doctors should explain the reasons for their choice of treatment in detail as this ensures a better understanding and closer following of guidelines. Listening to patients’ preferences and opinions and establishing a bidirectional relationship significantly improves adherence to treatment.