The study, published in the journal The Lancet Oncology, shows that all patients treated with this CAR T-cell product, developed at the hospital, had a response to the treatment. Almost 70% of the responses were complete after 18 months and the rest were partial. The research was supported by the Carlos III Health Institute and the “la Caixa” Foundation.
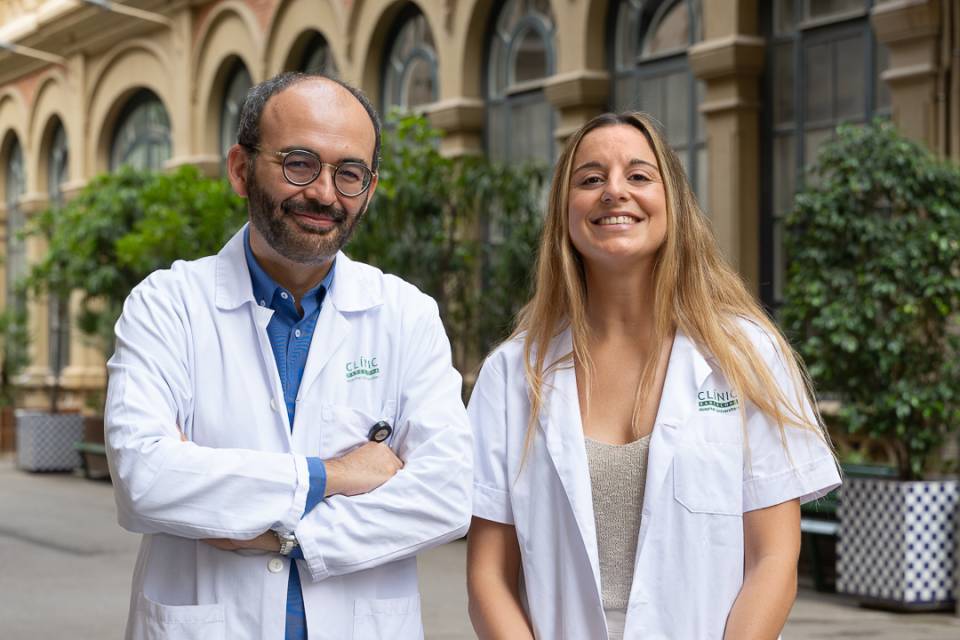
The coordinator of the study was Dr. Carlos Fernández de Larrea, haematologist at the Hospital Clínic and head of the IDIBAPS Myeloma, amyloidosis, macroglobulinemia and other gammapathies research group.
The development of CAR T-cell therapies at the Hospital Clínic has the fundamental support of the "la Caixa" Foundation, thanks to a strategic alliance to promote pioneering high-impact cancer research and to improve care for cancer patients. In order to carry out this clinical trial, specific funding was also received from the Carlos III Health Institute (ISCIII) and the Bosch Aymerich Foundation.
The trial was carried out in collaboration with the Clínica Universidad de Navarra, which collaborated with the professionals at the Hospital Clínic to produce this type of therapy, and three other Spanish hospitals: the Hospital Clínico Universitario de Salamanca, the Hospital Clínico Universitario Virgen de la Arrixaca in Murcia and the Hospital Universitario Virgen del Rocío in Sevilla.
First CAR T-cell therapy developed in Europe for multiple myeloma
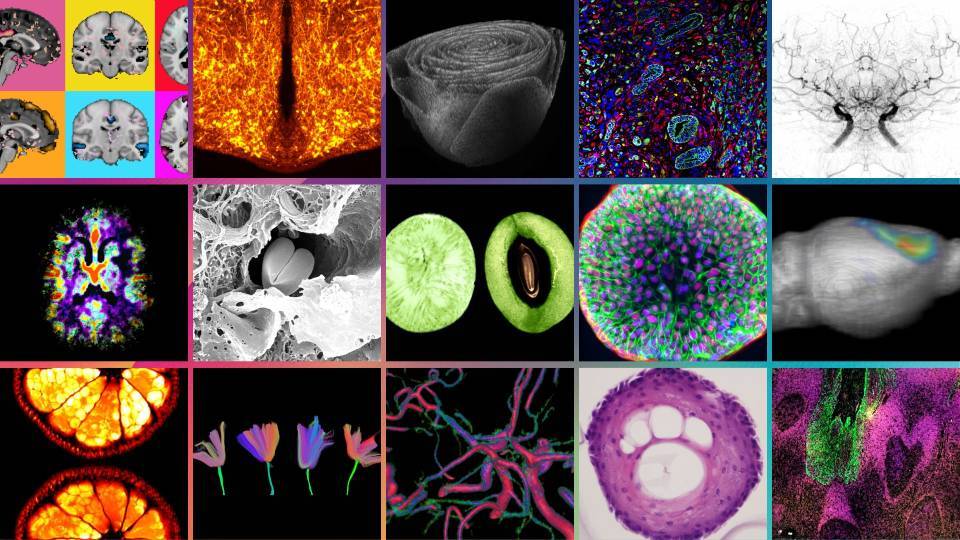
CAR (Chimeric Antigen Receptor) T-Cell therapy represents a promising option in the treatment of resistant multiple myeloma. It is a type of cell-based gene therapy in which the patient becomes his/her own donor. It consists of altering the patient’s T cells so that they are able to attack cancer cells.
CART T-cell therapy ARI0002h targets the BCMA antigen, which is found on the surface of myeloma cancer cells. Preclinical studies showed that ARI0002h was highly specific and effective against malignant multiple myeloma cells.
This is the second CAR T-cell therapy developed at the Hospital Clínic-IDIBAPS. “The difference with regard to previous CAR T-cell therapies, in addition to the therapeutic target, which in this case is the BCMA antigen, is that this time it is humanized. Mouse antibodies are often used to develop CAR T-cell therapies and in this case we humanized it in order to ensure it has greater durability in the patient and a lower probability of rejection”, explains Dr. Manel Juan, head of the Immunology Service at the Hospital Clínic, of the IDIBAPS Immunogenetics of the autoinflammatory response group, and in charge of the joint platforms at the Hospital Sant Joan de Déu and the Blood and Tissue Bank.
Dosing treatment to reduce toxicity
Multiple myeloma accounts for 10% of all bone marrow cancers. This is where the plasma cells (a type of white blood cell) responsible for producing the antibodies that help fight infections are found. In multiple myeloma, these plasma cells undergo an abnormal growth process and form tumours in the bones.
Patient survival has improved significantly thanks to the incorporation of certain treatments, although a significant proportion of patients relapse and generate resistance to the therapies. The Hospital Clínic-IDIBAPS team has developed a new CAR T-cell therapy product, ARI0002h, to treat these patients.
In order to assess the efficacy of CAR T-cell therapy ARI0002h, the Hospital Clínic-IDIBAPS started a trial with four other hospitals to treat 30 myeloma patients who had relapsed after two or three previous treatments. All the centres carried out apheresis to obtain the patients’ lymphocytes, and the CAR T-cell product was manufactured at the Hospital Clínic Barcelona and the Clínica Universidad de Navarra.
“Thanks to what we learned from previous trials with the CAR T-cell products developed at the hospital, we observed that administering the initial dose fractionally could reduce the severity of adverse effects without reducing efficacy”, explains Carlos Fernández de Larrea. “Thus, the first dose is administered in three aliquots and, 100 days after the first infusion, a booster dose is administered that provides a sustained response over time with low toxicity", he adds.
The results of the study published in The Lancet Oncology show that, after an 18-month follow-up, all patients responded to treatment and of these, 67% were complete responses, 27% were very good partial responses, and 7% were partial responses. At 3 months, no residual disease was identified in 24 of the 26 patients with bone marrow samples. Furthermore, no neurological toxicity was seen and immunological adverse effects were mild, thanks in part to the administration schedule.
Although the results are promising, patients treated with ARI0002h continue to relapse, requiring strategies to overcome this obstacle. “We have conducted studies that reveal that there are different mechanisms that could be responsible for the relapse after treatment with this CAR T-cell therapy. Moreover, we have detected that CAR T cells remain in the blood for five months and, although this time is similar to that of other CAR T-cell therapies for this disease, it is still short", points out Dr. Fernández de Larrea. “So, our research is aimed at finding out how we can extend the persistence of the CAR T-cell therapy”, he concludes.
In addition to the 30 patients participating in this study, another 30 patients were also added, including two other Spanish hospitals, and the treatment was administered on a compassionate use basis in 12 more patients.
Now, the Spanish Agency of Medicines and Medical Devices (AEMPS) is evaluating the documentation based on the results of this study for approval as a non-industrially manufactured advanced therapy medicinal product.
Study reference:
Oliver-Caldés A, González-Calle V, Cabañas V, et al. Fractionated initial infusion and booster dose of ARI0002h, a humanised, BCMA-directed CAR T-cell therapy, for patients with relapsed or refractory multiple myeloma (CARTBCMAHCB-01): a single-arm, multicentre, academic pilot study. Lancet Oncol 2023. https://doi.org/10.1016/S1470-2045(23)00222-X