In Western countries, cirrhosis is among the 10 leading causes of death among adults. It is a very common disease in Spain and the leading cause of liver transplantation in this country. It is responsible for a high rate of hospital admissions and use of health resources due to complications that occur in advanced stages of the disease.
Perverse repairing effect
Cirrhosis is a chronic lesion characterised by the accumulation of scar tissue (fibrous nodules), which alters the normal structure and function of the organ. Chronic hepatic lesions are caused mainly by alcoholism, hepatitis C, and increasingly by obesity.
The accumulation of scar tissue impedes blood circulation in the liver, thus leading to portal hypertension (the portal vein). To relieve the pressure in the vein, collateral blood vessels develop outside the liver. The problem is then two-fold, first because the liver receives even less blood, thereby causing greater damage to the organ, and second because the blood vessels are of poor quality (pathological angiogenesis).
“Hepatic cells try to repair liver lesions, but the way by which they do this turns out to be fatal for the organ. This is a loop that gets bigger and finally threatens the patient’s life. Also, the collateral blood vessels form varicose veins in the oesophagus and stomach of patients with cirrhosis; these veins are fragile and have a high tendency to burst, causing heavy bleeding that is difficult to stop,” explains Mercedes Fernández, from IDIBAPS and co-leader of the study. “This is why a treatment that regresses and/or prevents pathological veins —which is not currently available— would be efficient,” she adds.
A target named CPEB4
VEGF (vascular endothelial growth factor) is the main effector protein in the development of blood vessels. “All current drugs that aim to prevent neovascularisation are based on inhibiting VEGF or VEGF receptors, but the problem is that indiscriminate attack of this protein impairs the normal development of blood vessels, thus causing unbearable adverse effects,” explains Méndez, from IRB Barcelona.
In a previous study published in Nature Medicine, Méndez, together with researchers at the Hospital del Mar in Barcelona, had already discovered that CPEB proteins are involved in blood vessel development in pancreatic and brain cancer. Given the urgent need to identify new targets for pathological angiogenesis, Méndez and Fernández started collaborating to examine the role of CPEB4 in this process in the context of cirrhosis, a disease characterised by profound neovascularisation.
“The best about the study is that we demonstrate that the development of pathological blood vessels can be stopped by interfering with CPEB4 proteins while positive vascularisation remains intact,” says Méndez. The experiments in cells in vitro, in animal models, and in samples taken from patients with cirrhosis have revealed the molecular mechanisms through which the increase in CPEB4 favours the overexpression of VEGF in cirrhosis.
From cirrhosis to liver cancer
The researchers uphold that the repair cycle that the liver enters worsens the situation to the extent that the regeneration nodules, which show high levels of CPEB4, form liver carcinomas. In this context, the Spanish Association against Cancer (Asociación Española Contra el Cáncer (AECC)) has awarded more than one million euros to the Méndez-Fernández tandem, who, together with Jordi Bruix (IDIBAPS-Hospital Clínic), will work in a coordinated manner to unravel the role of this molecule and to propose a treatment forliver carcinomas, the main liver cancerand third cause of death by cancer worldwide, with a 5-year survival rate of less than 10%.
In parallel, Méndez’s lab at IRB Barcelona is working on a research project on CPEB4 inhibitors. Last year they resolved the structures of these proteins at the atomic level—the previous step to the computational design of inhibitors, which is being undertaken in collaboration with Modesto Orozco, at the same centre. Furthermore, and with the support of the Botín Foundation, Méndez has fine-tuned an assay to test CPEB4 inhibitors, with the aim to speed up the detection of molecules with the greatest therapeutic potential.
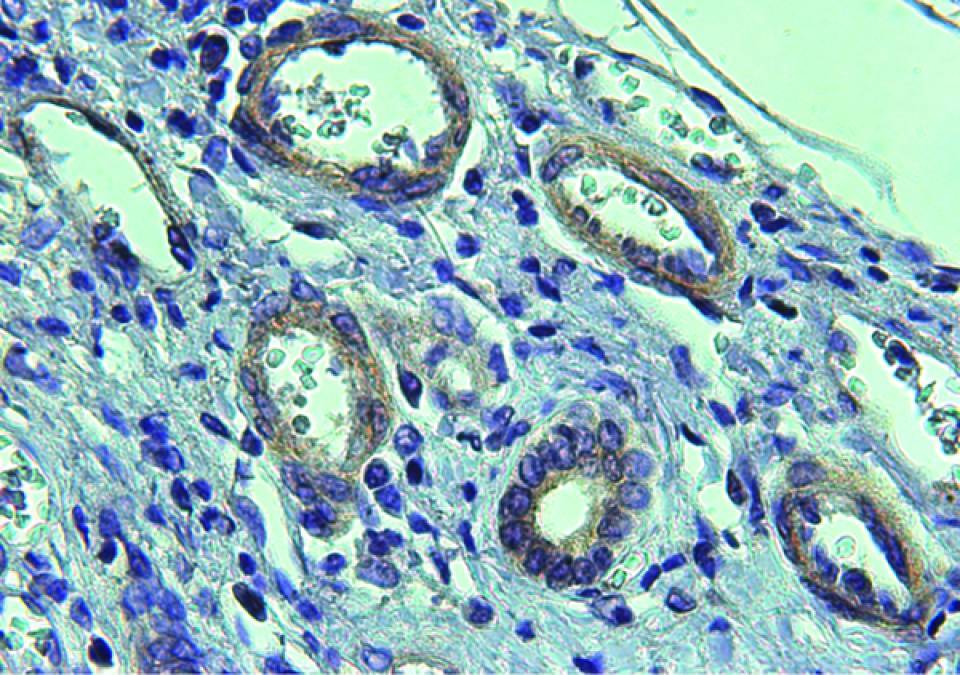
Image: Pathological blood vessels (white circles), with abundant CPEB4 expression in cirrhotic tissue (IRBBarcelona/IDIBAPS)
Reference article:
Calderone V, Gallego J, Fernandez-Miranda G, Garcia-Pras E, Maillo C, Berzigotti A, Mejias M, Bava FA, Angulo-Urarte A, Graupera M, Navarro P, Bosch J, Fernandez M*, Mendez R*.
Gastroenterology (2015). doi: 10.1053/j.gastro.2015.11.038