Chronic Hepatitis Delta affects between 15 and 20 million people worldwide, accounting for between 5% and 10% of all people infected with HBV. It is the most serious form of viral hepatitis, as it is associated with a higher risk of developing liver cancer and a shorter survival window compared to other forms of hepatitis.
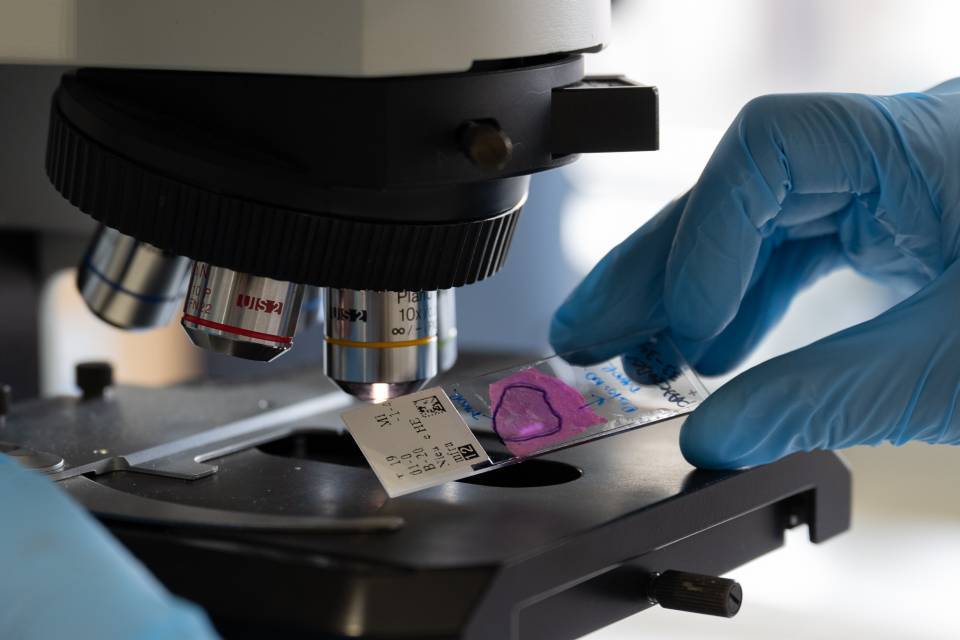
The study focused on the detection of two HBV markers: Hepatitis B core-related antigen and HBV RNA. These two markers are detectable in the blood and reflect the activity of a unique viral DNA called cccDNA, which is responsible for the production of all the components of HBV. This DNA is also highly stable in hepatocytes and cannot be eliminated with current HBV treatments. This is why the vast majority of patients with Hepatitis B receive treatment throughout their lives.
Recently published in the Journal of Hepatology and financed by CIBER, the study enrolled a large cohort of patients with untreated chronic Hepatitis Delta. Unexpectedly, the researchers observed a surprising pattern: most patients had no detectable HBV RNA in their blood, but they did have Hepatitis B core-related antigen. This is different than what is observed in Hepatitis B patients and suggests that HDV may be suppressing HBV replication.
This is a major discovery because HBV RNA and Hepatitis B core-related antigen are considered indicators of HBV activity in liver cells. The fact that HDV disrupts this balance could be key to understanding how this coinfection exacerbates the progression of liver disease.
‘Since HBV and HDV coexist in Hepatitis Delta, at first we would expect both factors, RNA and Hepatitis B core-related antigen, to be positive, as they reflect HBV replication. However, this wasn’t the case,’ says Sofía Pérez-del-Pulgar, a researcher in IDIBAPS’ Viral, genetic and immune mediated liver diseases research group, CIBER acreditated and one of the authors of the study. ‘We believe that the detection of only Hepatitis B core-related antigen could indicate the presence of empty capsids instead of actual viral particles with genetic material. This would suggest some previously unknown mechanism by which HDV interferes in the formation of HBV. Further studies will be required to understand how HBV and HDV interact and to clarify the pathogenic mechanisms involved’.