“These results confirm the potential for IPTi using SP, which can be easily and rapidly implemented via existing WHO immunisation programmes, saving tens of thousands of lives every year across Africa,” commented Dr. Clara Menéndez, principal investigator who lead the study. Dr. Pedro L. ALonso, head of the Secretariat of the IPTi Consortium at CRESIB (Hospital Clínic-Universitat de Barcelona), added: “IPTi provides a valuable addition to efforts to fight malaria and so international policy-makers and heads of national Malaria Control Programmes should consider its immediate adoption and integration into existing programmes”.
UNICEF’s Operational Research Coordinator, Dr. Alexandra de Sousa, stated “UNICEF supports IPTi implementation scale up in Africa, a new intervention in the control of malaria with the potential to significantly reduce child illness”.
A separate study in Northern Tanzania shows that in areas of very high resistance to the medication, IPTi with SP is not efficacious and alternative anti-malarial drugs are needed. The long-acting medicine mefloquine was seen to reduce the incidence of clinical malaria in infants in the first year of life by 38%. For the long term, it is important that research is accelerated to develop additional drugs for use with IPTi in different settings and in different circumstances, especially in areas where parasite resistance is a problem.
Malaria represents an important public health burden in Africa, disproportionately affecting the youngest and most vulnerable. Of the 247 million cases of malaria worldwide in 2006, 86% occurred in Africa, among which, African infants are at most risk of the worst forms of malaria. Every 30 seconds an African child dies from malaria.
About IPTi
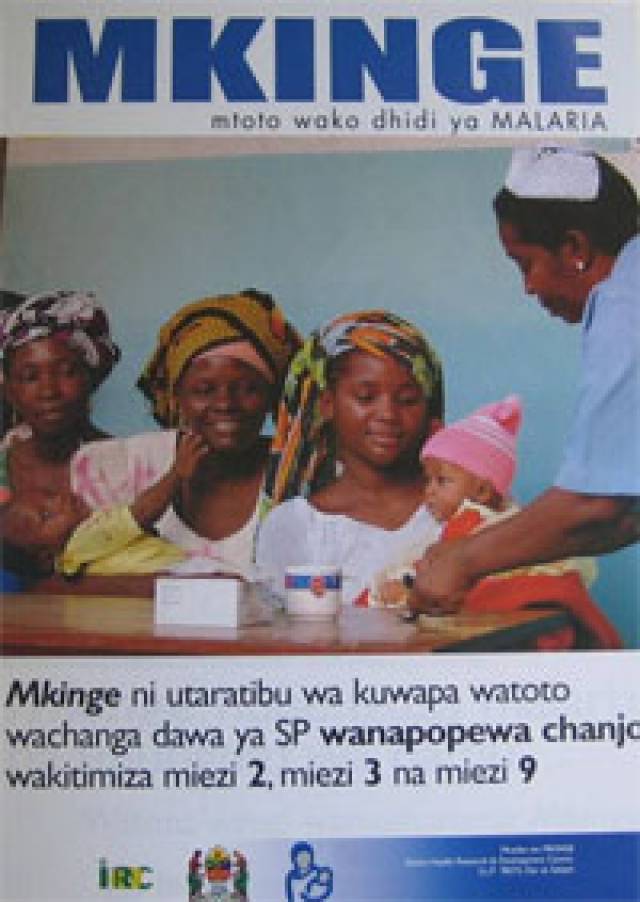
IPTi is the administration of an anti-malarial tablet to infants, two or three times in the first year of life, deliverable alongside established vaccination programmes such as WHO’s Expanded Programme for Immunisation. It is inexpensive (each dose costs between USD $0.13 - $0.23) and cost effective.
IPTi with SP has been reviewed by a committee of the US National Academy of Sciences’ Institute of Medicine and the World Health Organization’s Technical Expert Group – these committees recommend that it should be considered for implementation in areas of moderate to high levels of malaria transmission and low to moderate levels of parasite resistance to SP.
About the trials in the pooled analysis
Trials were conducted in Mozambique, Gabon, Tanzania and Ghana involving the following organisations in Africa and Europe: Barcelona Centre for International Health Research, Spain; Centro de Investigação em Saude de Manhiça, Mozambique; University of Tübingen, Germany; Ifakara Health Research Development Centre, Tanzania; University of Witwatersrand, Johannesburg, South Africa; Institute of Tropical Medicine and International Health, Charité, University Medicine Berlin, Germany; Kintampo Health Research Centre, Ghana Health Service/Ministry of Health, Ghana; London School of Hygiene and Tropical Medicine, London, UK; Albert Schweitzer Hospital, Lambaréné, Gabon; Ministry of Health/Ghana Health Service; Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany; Swiss Tropical Institute, Basel, Switzerland.
About the trial in Northern Tanzania
The trial was conducted in two sites in northern Tanzania, Korogwe and Same, by the following organisations; Department of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK; the National Institute for Medical Research, Tanga Centre, Tanga, Tanzania; and the Kilimanjaro Christian Medical College, Moshi, Tanzania.
About the IPTi Consortium
The IPTi Consortium’s Secretariat was the Barcelona Centre for International Health Research, Hospital Clinic, University of Barcelona, headed by Dr. Pedro L. Alonso. The IPTi Consortium consists of leading centres of malaria research in Africa, Europe, United States and Papua New Guinea including the Albert Schweitzer Hospital, Lambaréné, Gabon; Barcelona Centre for International Health Research, Hospital Clinic, University of Barcelona, Spain; Case Western Reserve University, Cleveland, USA; Centers for Disease Control and Prevention, Atlanta, USA; Ifakara Health Research and Development Centre, Ifakara, Tanzania; Institut de Recherche pour le Développement, Dakar, Sénégal; Kenya Medical Research Institute, Kisumu, Kenya; Kilimanjaro Christian Medical Centre, Moshi, Tanzania; London School of Hygiene and Tropical Medicine, London, UK; Manhiça Health Research Centre, Manhiça, Mozambique; National Institute for Medical Research, Amani, Tanzania; PNG Institute of Medical Research, Goroka, Papua New Guinea; Swiss Tropical Institute, Basel, Switzerland; Université Cheikh Anta Diop de Dakar, Dakar, Sénégal; University of Copenhagen, Copenhagen, Denmark; University of Tübingen, Tübingen, Germany; Walter and Eliza Hall Institute of Medical Research, University of Melbourne, Australia; World Health Organization (WHO); United Nations Children’s Fund (UNICEF).

