What is the risk of infection and transmission after receiving the vaccine?
The vaccine does not protect you against the virus entering your body or replicating initially within the mucous membranes. Those who are immunized can be infected and be asymptomatic or have a few mild symptoms, and can still be contagious.
The vaccines are 90% effective. Therefore, it is estimated that around 10% of those vaccinated may contract the virus and not develop immunity. This is more likely to occur in the elderly and in those with serious illnesses.
The cases of infection –despite having received the vaccine– are mild. In Catalonia, 0.12% of cases recorded were after the second dose, according to the Government of Catalonia’s COVID-19 data portal.
Moreover, those who have had COVID-19 develop a natural immunity, the duration of which is currently being studied. It is not known how long the antibodies remain to attack the virus after the infection. It has been observed that there are antibodies up to 39 days after the appearance of the initial symptoms. We speak of hybrid immunity when a person who has had the disease receives a single dose of the vaccine and can be immunized against even the most aggressive variants.
One dose, two doses, … third dose?
The first dose has a limited effect on the body. It stimulates the production of antibodies. However, the levels of the latter drop over time, and that is why a second dose is required, which stabilizes the levels for a longer period.
According to the disease prevention and control centres, the Pfizer vaccine requires the second dose 21 days after the first, and in the cases of Moderna and AstraZeneca, 28 days. Although an interval of 3-4 weeks is recommended, studies are still being carried out to evaluate the effectiveness of the vaccine depending on whether it is received before or after the recommended time.
Pharmaceutical companies Pfizer and BioNTech defend the option of the administration of a third dose. However, scientists argue that there is no scientific evidence to support this practice in people who have been fully vaccinated. Nonetheless, for transplant recipients, high-risk and immunocompromised people, it could work, because they generate between a third and half of the antibodies that healthy people produce after vaccination, due to the inhibition of their immune response as a result of the medication they take. However, Israel has already started to offer a third dose of the vaccine to this population group.
Vaccination coverage of 70% of the population and no more?
With 70% of the population vaccinated, the virus dies out naturally. So, it is the only way to stop the pandemic. The current vaccines are effective, but not perfect, because people can get infected and spread the virus.
Research into new treatments, vaccination, and the evolution of the disease with the different variants are ongoing, and thus preventive measures are still being taken: washing hands frequently, prioritizing outdoor spaces, practising physical distancing for safety, continuing to use a mask, having diagnostic tests if you have been in contact with a person who tests positive for COVID-19, and strictly respecting isolation periods.
Many epidemiologists insist that carrying out more accurate screening and rapid antigen testing on a massive scale would make a substantial difference in terms of controlling the disease and the rate of infection.
Why are new variants produced?
Viruses, like any species, fight to survive and therefore change to adapt to their environment. Many random mutations can occur in the virus, most of which will have no effect. However, others will work and enable it to adapt better to its environment, allow it to overcome barriers and then enter our cells and replicate.
The human body also adapts to the external threats it encounters. Lymphocytes are the cells that produce antibodies and, when they recognize the virus, they act to eliminate it. These lymphocytes undergo somatic hypermutation, with many variants being produced in order to recognize new versions of the virus and to adapt.
The variants that generate the most interest are those that develop mutations in the gene that codes for the S protein, since it can lead to changes in the virus’ infectivity and in the immune response of the vaccines. The British, South African and Indian variants are more transmissible, due to mutations in this gene. With the Delta variant, the effectiveness of the vaccine is not sufficiently known, but a recent study in the New England Journal of Medicine explains that vaccination provides 95% protection against the new strain, provided that the two doses are given.
In epidemiology, the number of new cases that an infected person generates is known as the basic reproductive number (R0). In the case of the Delta or Indian variant, 1 infected person passes the virus on to 4 people, whilst with the Wuhan variant, 1 infected person generated 2.5 infections. "The new variants seem more contagious, but they do not cause more serious disease,” says Dr. Manel Juan, head of the Immunology Service at the Hospital Clínic de Barcelona.
Can the safety of the COVID-19 vaccine be called into question, due to the fact that it was manufactured rapidly?
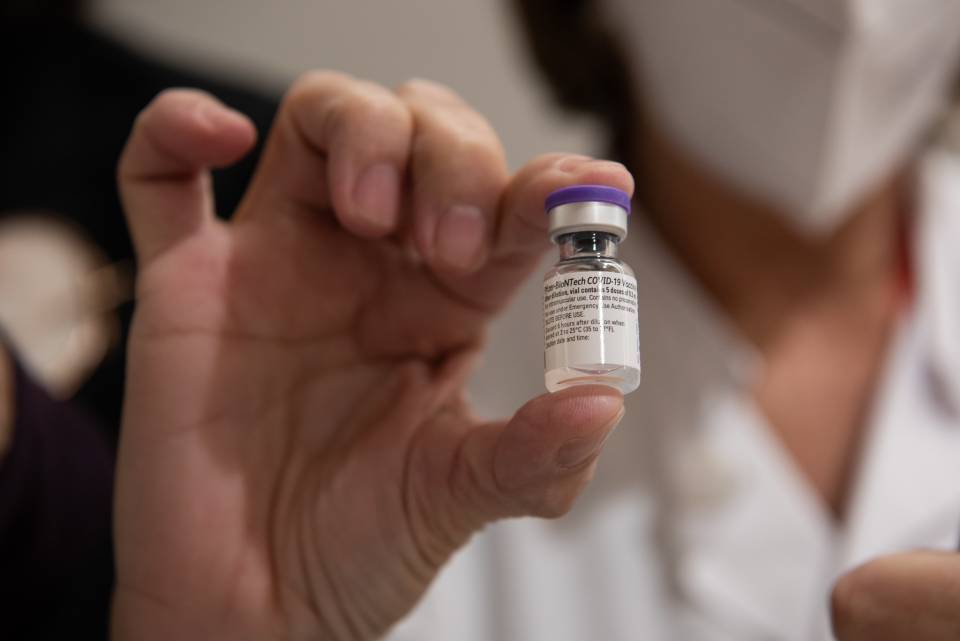
The Pfizer / BioNTech, Moderna, Oxford / AstraZeneca and Janssen vaccines are those that have been authorized by the European Union to combat COVID-19. They are Phase III vaccines, and they have been shown to produce no serious side effects. So, they can be considered safe. However, due to the speed at which the clinical trials were conducted, we still do not know how long they provide protection for.
"The speed at which they were manufactured is due to the fact that significant financial resources were invested, and processes were carried out in parallel. A new phase started before the previous one finished,", comments Dr. Felipe García, internist in the Infectious Diseases Service at the Hospital Clínic de Barcelona.
The process required to obtain a vaccine consists of preclinical studies, which are carried out using animals. They check that the animals are not infected after receiving the vaccine and that they develop defences. Clinical trials are then conducted with people, and these involve several phases. In Phase I, several dozen volunteers are vaccinated in order to find out the correct dose and ensure it is safe. In Phase II, hundreds of individuals are tested to check the safety of the vaccine and its ability to induce an immune response. In Phase III, the vaccine is given to thousands of individuals (30,000 – 40,000). Finally, in Phase IV, the pharmacovigiliance (safety surveillance) phase, the vaccine’s effectiveness is studied once it is on the market.
What are the differences between the existing vaccines?
The vaccine must always guarantee the detection of the virus and prevent the person from getting ill. Since all the vaccines perform this dual function, they are considered equally effective.
Pfizer and Moderna are messenger RNA (mRNA) vaccines, which encode segments of a protein in the SARS-CoV-2 virus, the S protein (spike), a transmembrane protein that enables the virus to bind to our cellular receptors and infect us. These vaccines contain genetic material synthesized in a laboratory, which make the cells produce copies of the S protein, or spike. This stimulates our immune response, as the body recognizes this protein as foreign and specific antibodies are generated. So, if the body encounters the virus, it will be better able to defend itself.
The AstraZeneca vaccine consists of a replication-deficient chimpanzee adenovirus vector, which contains the genetic sequence of the S protein.
Janssen is a human adenovirus vector-based vaccine and carries the genetic code for the same protein. Adenoviruses are DNA viruses that, using genetic engineering, are modified in the laboratory in order to make them replicate and express the protein we are interested in.
Which new vaccines and drugs are currently in the pipeline?
The Spanish National Research Council (Centro Superior de Investigaciones Científicas, CSIC) is developing a new vaccine that is expected to be ready in a year’s time. It will be administered through inhalation, which guarantees local protection of the respiratory tracts and of the virus’ main point of entry. Unlike the current vaccines, it will provide sterilizing immunity, preventing people getting ill and infecting others, which makes it the most promising vaccine developed to date. In addition, the mutations of the SARS-CoV-2 variants from the United Kingdom, South Africa and Brazil have been incorporated.
Few antiviral drugs can be used and they have many adverse side effects. Moreover, there are antibodies that could be incorporated into the body to stop the disease. However, they are very expensive and are hard to administer on a mass scale. For the moment, there is no specific drug to treat SARS-CoV-2. However, it is hoped that research is heading in the right direction and will result in efficient antiviral treatments to tackle this global public health challenge of the 21st century.