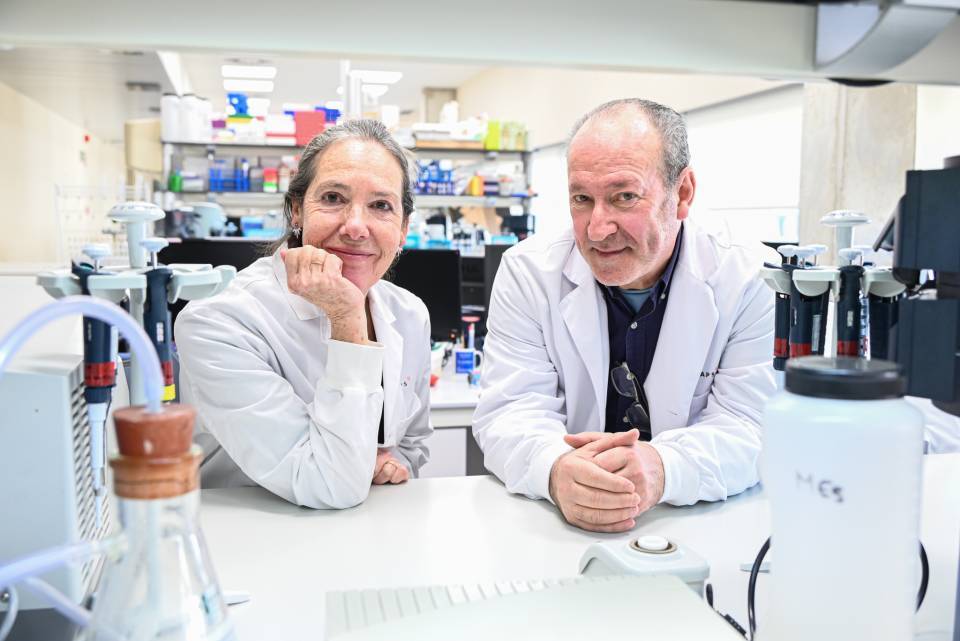
This project is coordinated by the Sandford Burham Prebys Medical Discovery Institute (SBP, California) and is jointly led by José C. Fernández-Checa, a IIBB-CSIC researcher and the head of the IDIBAPS research group Mitochondrial regulation of cell death and steatohepatitis, and Neil Kaplowitz, from the University of Southern California (USC), in one of the three projects into which the study is divided. The global PO1 programme consists of three research projects and three cores and has received over 13 million dollars in total funding (total costs).
Hepatocellular carcinoma is one of the most common forms of liver cancer and a primary cause of cancer-related death worldwide. Non-alcoholic steatohepatitis is the most prevalent liver disease in the world and a leading cause of hepatocellular carcinoma. This five-year NIH-funded project suggests that metabolic reprogramming due to hypernutrition accelerates the progression of non-alcoholic steatohepatitis to liver cancer.
‘This project provides a unique opportunity to define how energy diets affect the regulators that promote the progression of NASH to hepatocellular carcinoma, creating new preventive and therapeutic strategies’, José C. Fernández-Checa says.
The full programme consists of three projects. The first two, led by Michael Karin from the University of California San Diego and Randal Kaufman from the SBP, will study how alterations in the metabolism of cholesterol and other lipids, as well as the consequent oxidative stress and impact on the functions of the endoplasmic reticulum (a cellular organelle), encourage the appearance and progression of hepatocellular carcinoma. The third project, which is co-led by IDIBAPS and will be carried out at the CSIC facilities, aims to decipher the molecular mechanisms by which two proteins resident in mitochondria (STARD1 and SAB) facilitate the onset of liver cancer. This third project has received more than two million dollars in funding.
It is believed that mitochondrial dysfunction accentuates changes in the metabolism of cholesterol and oxidative stress, leading liver cells to a state of senescence that aids in the accumulation of mutations and, therefore, the appearance of cancer. Overall, it is thought to behave in a kind of spiral feeding back on itself that facilitates and accelerates the carcinogenic process.
‘For our part of the project, we will integrate the metabolic changes discovered in parts 1 and 2 with the mitochondrial alterations potentially causing liver cancer’, Fernández-Checa explains. ‘Interference with key components of this network may suppress the progression of cancer and give rise to new therapeutic strategies’.