The connection between hypothalamus and pancreas
POMC neurons detect changes in nutrient availability, but the molecular mechanisms involved are not known in detail. Also changes in the shape of mitochondria, a phenomenon known as mitochondrial dynamics, is a mechanism of energy adaptation in changing metabolic conditions, to adjust the needs of cells.
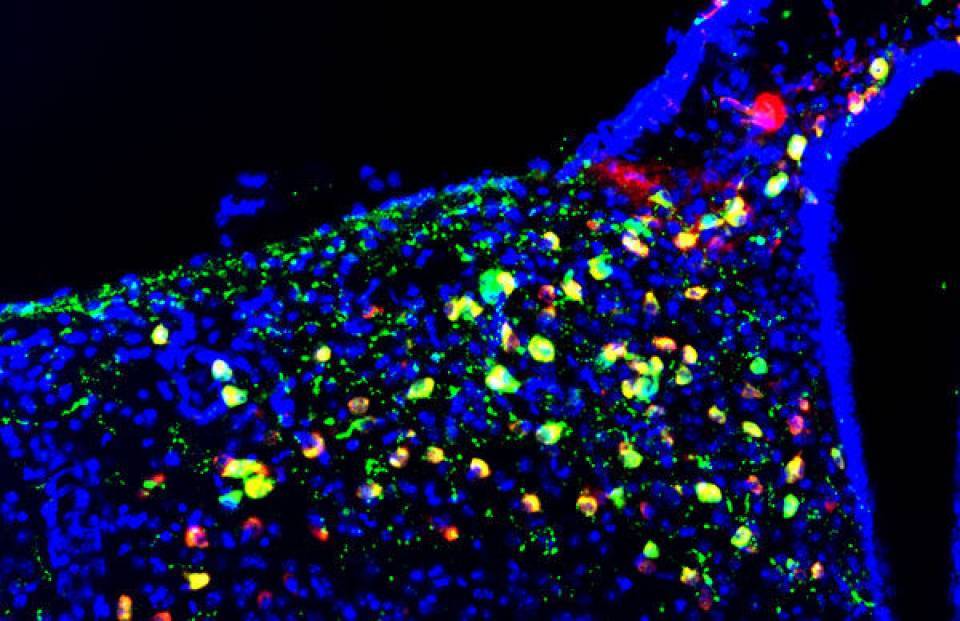
To determine whether defects in the mitochondrial dynamics of this small nucleus of POMC neurons could cause alterations in metabolism, researchers removed a mitochondrial dynamics protein, Mitofusin 1, in these cells in mice.
First, the scientists observed that these mice have altered detection of glucose levels and adaptation between the fasting state and after being fed. Second, they found that these defects lead to disturbances in the glucose metabolism that are caused by a lower secretion of insulin. "It was surprising to discover that these neurons are involved not only in the control of the intake, which was already known, but also in the control of the amount of insulin secreted by the beta cells of the pancreas," explains Zorzano, Head of the Laboratory of Complex Metabolic Diseases and Mitochondria at IRB Barcelona.
Scientists observed for the first time that this communication between the hypothalamus and the pancreas depends on the activity of the protein Mitofusin 1 and are starting to understand some molecular details of this connection. They describe that the alterations are due to a disproportionate, though transitory, increase in the production of radical oxygen species (ROS) in the hypothalamus. When the levels of ROS in the hypothalamus are restored in the laboratory, the pancreas starts to secrete the correct levels of insulin again.
Obesity and diabetes
Marc Claret, head of the Neuronal Metabolism Control Group at IDIBAPS, adds that "our results also suggest pathological implications of this animal model, since a diet rich in fats makes these mice more susceptible to developing diabetes."
Insulin segregation is a major phenomenon in relation to diabetes. Type 2 diabetes patients, who represent the 85% of people with diabetes, have fewer beta cells and less ability to secrete insulin in response to glucose. "Understanding the mechanisms involved in regulating insulin is important and therefore helps us to better understand the pathophysiology of diabetes," says Claret, who emphasizes that "much research needs to be done to apply these findings, given that we are talking about neural mechanisms of complex intervention."
This work has been funded by the Spanish Ministry of Economy, Industry and Competitiveness and the European Research and Development Funds (ERDF). The study involved researchers from the Yale School of Medicine (US), the Faculty of Medicine of the University of Geneva (Switzerland), the University of Barcelona, the Paul Sabatier University of Toulouse (France), the University Hospital Virgen del Rocío in Seville, the University of Santiago de Compostela, the Bellvitge Biomedical Research Institute (IDIBELL), the University of Veterinary Medicine (Hungary) and the Hospital Clínic of Barcelona.
Reference article:
Sara Ramírez, Alicia G Gómez-Valadés, Marc Schneeberger, Luis Varela, Roberta Haddad-Tóvolli, Jordi Altirriba, Eduard Noguera, Anne Drougard, Álvaro Flores-Martínez, Mónica Imbernón, Iñigo Chivite, Macarena Pozo, Andrés Vidal-Itriago, Ainhoa Garcia, Sara Cervantes, Rosa Gasa, Ruben Nogueiras, Pau Gama-Pérez, Pablo M Garcia-Roves, David A Cano, Claude Knauf, Joan-Marc Servitja, Tamas L Horvath, Ramon Gomis, Antonio Zorzano and Marc Claret
Cell Metabolism (2017). doi: 10.1016/j.cmet.2017.05.010