Despite the progress achieved over the last decades, malaria is estimated to have caused almost half a million deaths in 2016, mostly among children. The definition of severe malaria was established to identify those children at risk of dying, but in reality it is a complex and heterogeneous disease that not always responds to the recommended treatments.
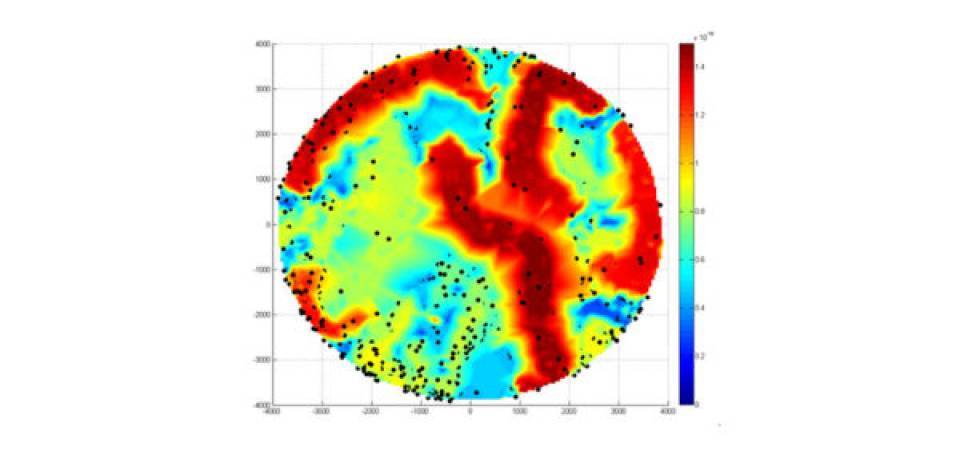
The team led by Climent Casals-Pascual, researcher at ISGlobal-Hospital Clínic and at Oxford University, applied a computational analysis based on networks in order to identify biologically relevant phenotypes apart from those currently defined by the WHO (cerebral malaria, respiratory distress, and severe malarial anaemia). For this, they performed a ‘network-based clustering analysis’ with data from almost 3,000 Gambian children hospitalized with malaria. They found that the mortality was higher in those clusters with higher phenotypic heterogeneity. The analysis revealed four clusters of patients with both respiratory distress and severe anaemia, in which an enlarged liver was associated with higher mortality. By analysing plasma proteins of these patients, they showed that this is likely due to heart failure.
“Our results indicate that heart failure should be reconsidered as a pathogenic mechanism in severe malaria,” explains Casals-Pascual, “and that therefore the standard clinical management may not be appropriate for these patients”. This type of “systems approach” can be a very valuable tool to identify new phenotypes and mechanisms as well as therapeutic options for complex diseases”, he adds.
Reference
Cominetti O, Smith D, Hoffman F, et al. Identification of a novel clinical phenotype of severe malaria using a network-based clustering approach. Scientific Reports. 2018. 8:12849. DOI:10.1038/s41598-018-31320-w