What is a Pacemaker?
A pacemaker is a stimulation system that generates electrical pulses delivered by electrodes; it is implanted in the heart and connected to a battery. The battery generates electrical pulses and works as a pacemaker generator.
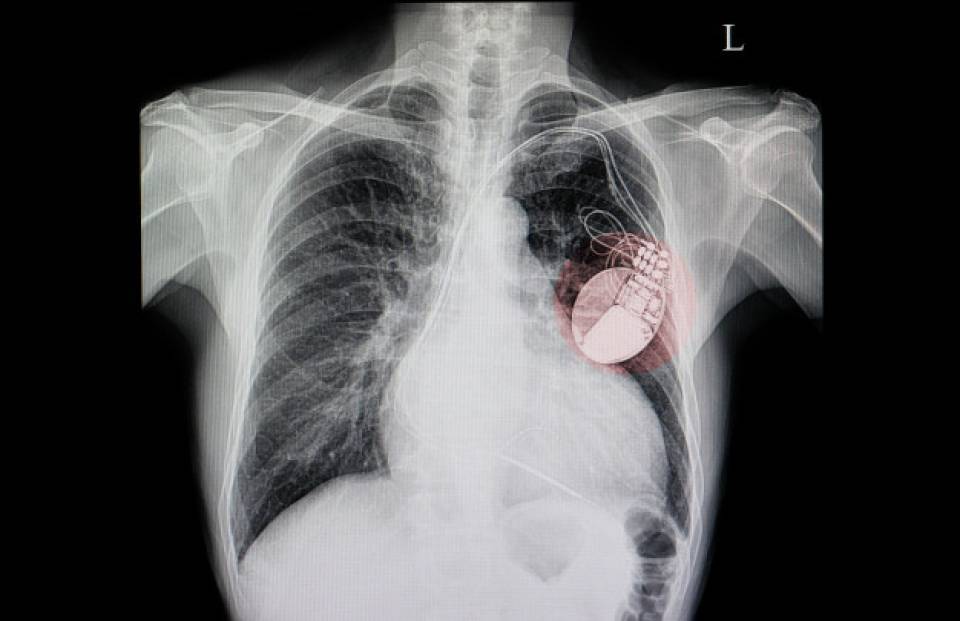
The pacemaker is implanted at chest level, under the skin or muscle. It is made of titanium and is designed to control the heart rate. Depending on the pathology, a pacemaker has 1, 2 or 3 electrodes connected to it. Currently, there are pacemakers that have an integrated lead and are like a small capsule implanted directly into the right ventricle of the heart, known as transcatheter pacemakers.
When is a pacemaker necessary?
A pacemaker is needed when there is a disturbance in the heart rhythm due to a disease of the conduction system in the heart. This means the electrical current is either not transmitted or inadequately so, leaving the heart unable to beat properly. Some of the heart problems that may require a pacemaker are:
-
Sinus node dysfunction: the part of the heart where the electrical impulse originates does so with insufficient frequency.
-
Atrioventricular block: the electrical current from the atria to the ventricles is partially blocked or completely, with no conduction.
Both pathologies manifest as a slow, irregular heartbeat or one with long pauses (asystole).
There are also some patients with heart failure who have an uncoordinated heartbeat that contracts the heart with little force. In these patients, a pacemaker can stimulate both the left and right ventricles and help to coordinate the beats, improving cardiac function and the symptoms associated with heart failure. This is called cardiac resynchronisation therapy.
Types of Pacemakers
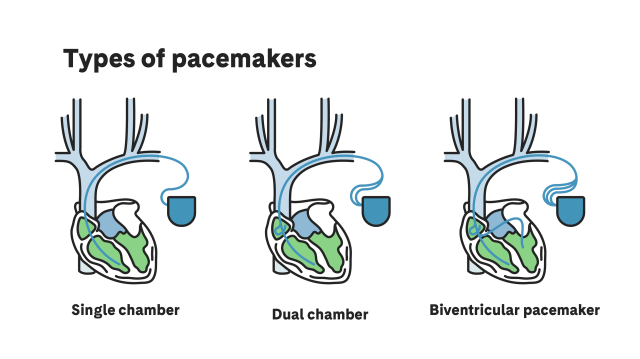
There are different types of pacemakers, depending on the cardiac chamber to be detected or stimulated:
-
Single chamber: An electrode (a thin insulated wire) detects the signals and provides electrical impulse to a single chamber of the heart. This may be in the right atrium or right ventricle.
-
Dual chamber: This has 2 electrodes that detect the signals and give electrical impulses to 2 heart chambers; coordinating the right atrium and right ventricle.
-
Biventricular: This has a third electrode that gives an electrical impulse to the left ventricle, synchronising it with the right ventricle.
Preparation for implantation
The following is needed before the operation:
-
Fasting for a minimum of 6 hours.
-
Having the chest area and armpits shaved.
-
For those undergoing anticoagulant or antiplatelet treatment, there are different protocols depending on the risk of thromboembolism or bleeding. Ideally, the arrhythmia unit should be consulted for the required instructions.
How is it performed?
The pacemaker is surgically implanted, usually on an outpatient basis; therefore, the patient can go home the same day. The procedure is performed under local anaesthesia and light sedation to make it more comfortable for the patient.
-
An intravenous antibiotic is administered to prevent infection.
-
The electrodes to be implanted are inserted through the axillary or subclavian vein. These veins are located below the armpit and collarbone, and accessed through either, depending on the needs of the patient.
-
An incision is made 5-10 cm below the collarbone to create a space for the pacemaker to be fitted.
-
The required electrodes are placed inside the heart and tests are carried out to confirm that the signals from the heart are detected and that it is pacing properly.
-
The device is inserted under the skin. The electrodes are attached to the muscle to stop them from moving.
-
Leads are attached to the pacemaker.
-
The thoracic incision is closed with absorbable sutures and staples.
-
A hydrocolloid dressing is applied to help heal the wound.
-
The pacemaker is programmed according to the patient needs.
-
A compression bandage is applied to prevent bleeding and possible bruising afterwards.
The access route for a transcatheter pacemaker is the femoral vein. It is also performed under local anaesthesia with light sedation.
-
A catheter is inserted through the femoral vein, located near the groin.
-
The catheter carries the transcatheter pacemaker into the right ventricle.
-
The device is installed in the heart wall and attached with flexible ties.
-
Checks are made to confirm that the heart signals are being detected and that they are pacing properly.
-
The catheter is removed.
-
A compression bandage is applied to the area of the femoral incision to prevent bleeding and, later, bruising.
Where is it performed?
Currently, the Hospital Clínic Barcelona has 3 electrophysiology rooms where most pacemaker implants are performed. In exceptional cases, they are carried out in cardiovascular surgery operating rooms.
Who performs the operation?
The operation is conducted by the unit's medical team with external nursing support from the arrhythmia unit. This team usually has 1 electrophysiologist and 1 arrhythmia nurse.
Depending on the device to be implanted, sometimes there may also be help from the device manufacturer's technical services.
How long does it take?
The procedure can take between 1 and 3 hours, depending on the device to be implanted.
What will I feel during and after the Pacemaker implant?
There may be pain in the implant area during and after the device is fitted, which will decrease with painkillers. Palpitations may also be felt, caused by the electrodes being inserted into the heart.
Once the pacemaker is functioning, the patient can lead a normal life and the symptoms for which the device was implanted (e.g., dizziness and fatigue) should resolve themselves. Thus, the health and quality of life of the person fitted with the pacemaker will improve.
A hydrocolloid dressing will be applied and will need no further attention. It must be kept on until the scheduled visit 10-15 days after the operation. This dressing will change its colour and appearance, but that is part of the healing process. However, if there is fluid leakage outside the dressing, the medical team must be consulted to make an assessment.
Pacemakers require routine monitoring to verify their proper functioning and condition. This is done by advanced practice nurses. Checks are carried out in person or with remote monitoring for better detection of any problems with the device.
What are potential complications?
Complications with the implant or replacement of the pacemaker can occur in up to 10% of cases. However, most of these complications can be resolved easily by reprogramming the device or other simple measures. A small percentage of patients require a second operation.
There may be acute complications or others related to the implant or replacement procedure. These occur in the first few days or weeks after the operation; examples are bruising in the wound (more frequent in patients with antithrombotic or anticoagulant treatment); infection (more frequent in pacemaker replacements than actual implants); dislodging of the electrodes; or, more seriously, cardiac perforation.
In the long term, the proper condition and operation of the device (electrodes and generator) must be checked. Over time, the implanted electrodes can wear out and fracture, causing the device to malfunction. If this happens, new electrodes must be implanted by operating on the patient again. Recently, remote monitoring of patients has been made possible by a device that transmits possible alerts to a hospital platform, for faster detection of complications.
Related contents
Substantiated information by:



Published: 22 March 2023
Updated: 22 March 2023
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox