- Gynaecological Ultrasound
- Team and structure
What is Gynaecological Ultrasound?
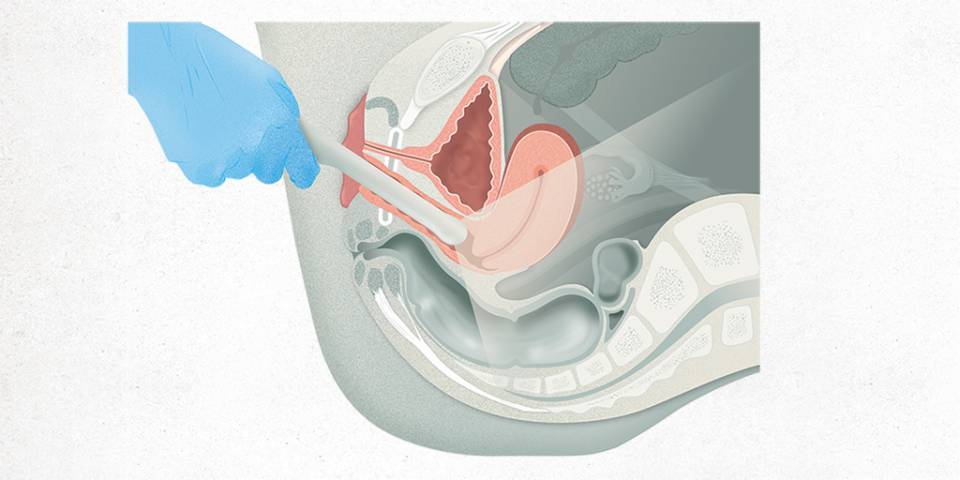
A gynaecological ultrasound is a diagnostic test used to view the pelvic organs (uterus or womb, ovaries, bladder and rectum or final portion of the large intestine) using an ultrasound probe placed inside the vagina (transvaginal).
A transvaginal probe allows the internal genitalia to be examined very detailed, as it comes very close to the area. Furthermore, better resolution is achieved transvaginally than with an abdominal probe (like those placed on the belly during pregnancy).
This type of scan uses ultrasound to produce an image. It does not emit any radiation. This means as many ultrasounds as necessary can be performed without having any negative effect on the patient.
In addition, it is a dynamic test: it is interpreted in real time, as it is performed. It allows the movement of the organs and the relationship between them to be observed (whether or not they are attached, for example), as well as allowing painful areas to be identified.
When is a gynaecological ultrasound necessary?
Generally, a gynaecological ultrasound is performed to discard a visible disease of the internal genital organs (uterus or womb, fallopian tubes or ovaries).

For example, if a woman has very heavy menstrual bleeding, a gynaecological ultrasound can rule out the presence of polyps or fibroids (benign tumours in the uterus), or may indicate a malignant uterine tumour.

With abdominal pain around the pubis or on both sides, an ultrasound scan can identify whether there are ovarian tumours (both benign and malignant).

If menstruation is very painful, this test will show whether the pain is caused by diseases such as endometriosis.

If a woman’s periods are irregular or widely spaced, ultrasound can help diagnose the cause (hormonal disturbances or premature ovarian ageing).

Some gynaecological diseases also affect the bladder, urethra or bowel wall, all of which can also be identified. For example, endometriosis is the presence of endometrial cells (from inside the uterus) outside the uterine cavity. They can be found for example in the ligaments connecting the uterus to the sacrum, in the large intestine and the bladder wall; these structures are visualized by gynaecological ultrasound.
Other uses of an ultrasound include assessing how a mesh is positioned under the urethra to treat urinary incontinence, or examining some anatomical features of women with vaginal prolapse (descent) of the organs.

We sometimes perform gynaecological ultrasounds to rule out pathology in women who have no symptoms but are at risk of developing a disease, as a form of screening. For example, women who have a genetic alteration that increases their risk of uterine or ovarian cancer.

Gynaecological ultrasound is the test of choice for studying the pelvic anatomy of women with difficulty conceiving, both to rule out disease and to assess certain parameters of response to reproductive treatments, such as ovarian reserve.
What preparations are needed?
A gynaecological ultrasound normally does not require any preparation. When examining the uterus using an abdominal probe, the bladder should be full of urine to facilitate identification; but when done vaginally, it is preferable for the bladder to be empty.
In some cases, when the walls of the lower part of the large intestine (the rectum) need to be examined in detail, a simple bowel preparation is requested for the test: a low-fibre diet and an enema the day before the ultrasound. It is only requested for certain patients and detailed information is always provided before the test.
On other occasions, some kind of substance is introduced into the uterus to visualise the course of the tubes. In these cases, the patient should take an antibiotic prior to or after the test as a preventive measure to avoid possible infections.
How is it done?
The patient undresses from the waist down, as she does when she has a gynaecological examination. The patient positions herself as follows: lying on her back with her legs apart, with the legs placed on a special support on the examination bed. For greater privacy, the waist is covered with a towel or dressing gown.
Then, the health professional (usually a gynaecologist) inserts the probe into the vagina. The probe is a long, narrow instrument that measures less than 2 cm in diameter. It emits ultrasound waves and is connected to the ultrasound machine. The probe is inserted into the vagina with a protective latex sheath (similar to a condom), and covered with a gel that both lubricates and acts as a conductor of the ultrasound waves to help obtain a high quality image. Then the pelvic organs are displayed on the screen, and the medical professional moves the probe around to be able to identify, assess and measure them.
A gynaecological ultrasound is an ultrasound scan of the internal genitalia examined from the vagina. If it cannot be performed vaginally, a very similar image can be obtained transrectally. The image of the genitalia obtained using an abdominal probe has a much lower resolution.
Pelvic floor ultrasound, which is indicated for women with urinary or anal incontinence, or pelvic organ prolapse (descent), is also performed by placing the probe on the vulva lips (translabial ultrasound).
In some cases, biopsies or punctures of different structures can also be performed during a vaginal ultrasound. A device is attached to the probe that allows a needle to enter, so that when the ultrasound probe is introduced into the vagina, it serves as a guide to puncture/inject a substance into the uterus, ovaries, or into the spaces between the uterus and the bladder or rectum.
Once the test is completed, the patient can get dressed again, and the health professional will interpret the test. They will usually make a report immediately and is available on the centre's computer system and the ‘La meva salut’ (My Health) app.
Where is it done?
Gynaecological ultrasound scans are performed at gynaecological practices equipped with beds with supports that allow the woman to assume the correct position for the examination.
Many gynaecological practices have ultrasound scanners to allow them to conduct complete assessments. There are also specialised ultrasound consultations, where more experienced ultrasound specialists examine patients who are suspected to have a specific pathology.
Who performs the test?
Unlike other radiological tests, gynaecologists perform gynaecological ultrasound scans. They also interpret the test and make reports.
Learning this technique is a key part of training as a gynaecologist. This is a very useful tool for monitoring both gynaecological conditions and pregnancy. .
How long does it take?
In general, the test takes no more than 5 minutes. In cases of complex pathology, it may be extended to 10 or a maximum of 15 minutes.
If any type of contrast dye needs to be introduced, or a biopsy or puncture is to be performed, the test may take longer due to the preparation needed for these procedures.
What will I feel during the test?
A gynaecological ultrasound is not normally a painful test.
When the vaginal probe first makes contact with the vulva, the patient will feel a cold sensation due to the gel put on the probe. As the probe is inserted into the vagina, the patient may feel some pressure until the instrument passes beyond the entrance of the vagina (depending on the width of the individual woman’s vagina). Once the probe has been placed inside the vagina, the gentle movements made to explore the different pelvic organs are usually painless.
Pressure is put on both ovaries to examine them in detail, which can be uncomfortable.
For women experiencing pain during penetration in sexual intercourse, or women who have ovarian or uterine lumps or pelvic infections, examining these structures may be painful. This is usually done as gently and as quickly as possible.
Contrary to popular belief, a transrectal ultrasound exam is not painful at all, as the probe is thin and the anal canal can adapt easily.
Our professionals are attentive at all times to patient comfort, so the test can be stopped or the pressure or movement of the probe reduced.
What are the possible complications?
In general, gynaecological ultrasound is a virtually harmless test, as the ultrasound frequencies that the equipment emits and the short exposure time does not produce any harmful effects to the body.
Introducing the probe into very narrow vaginas may cause some small lacerations at the opening of the vagina; if the probe comes into contact with cervical tumours it may cause bleeding; and examination of the pelvic organs in women who have previously experienced pelvic pain may temporarily intensify the pain.
If the probe cannot be inserted into the vagina due to pain or a narrow vaginal opening, the transrectal approach will be suggested. If this is not possible or the patient does not wish it, the test will not be performed, and other imaging tests that also identify the pelvic organs, such as a CT scan or MRI, will be considered.
The chance of transmitting infections via the test is practically non-existent, as the probe is sterilised and covered with a latex sheath.
If the ultrasound is performed to guide punctures or introduce/inject substances, the potential complications would be those typical of these procedures (bleeding, infections). These complications are also very uncommon and unlikely.
Substantiated information by:

Published: 25 January 2022
Updated: 26 May 2025
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox