What is a Fusion Prostate Biopsy?
A fusion prostate biopsy is an outpatient procedure to take a sample which is then used to diagnose or rule out prostate cancer.
A fusion prostate biopsy is a procedure to obtain samples of the prostate which combines images of the prostate from MRI and ultrasound. It provides 3-D images of the prostate which makes it easier to locate lesions described in the MRI. Samples of the prostate are taken with a needle from the indicated areas.
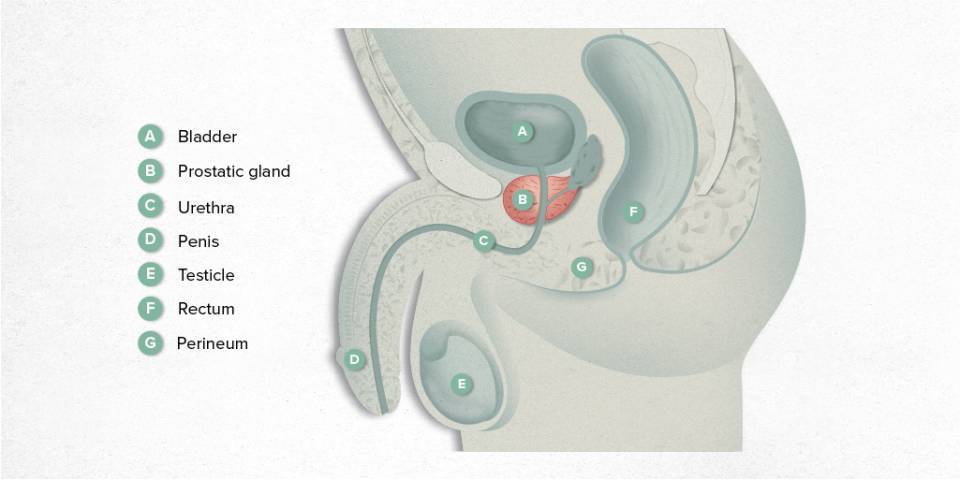
A man may be suspected of having prostate cancer if he has an abnormal prostate-specific antigen (PSA) level, a suspicious digital rectal examination or prostate magnetic resonance imaging (MRI) that indicates there may be a lesion in the prostate. To make the diagnosis, samples of the prostate are taken with an ultrasound-guided needle.
How is it performed?
Before a fusion prostate biopsy is performed with MRI-ultrasound, an earlier MRI scan of the prostate must have indicated a suspicious area in the prostate. Prostate lesions seen in MRI are classified according to the degree of suspicion, using a system called PI-RADS. If there is an indeterminate or suspicious lesion seen on the MRI, it is considered whether a targeted prostate biopsy should be performed.
Devices that perform fusion prostate biopsies have a program to capture MRI images of the prostate and superimpose them over transrectal ultrasound images in real time. This provides 3-D images of the prostate, which make it easier to locate suspicious lesions for sampling with a needle.
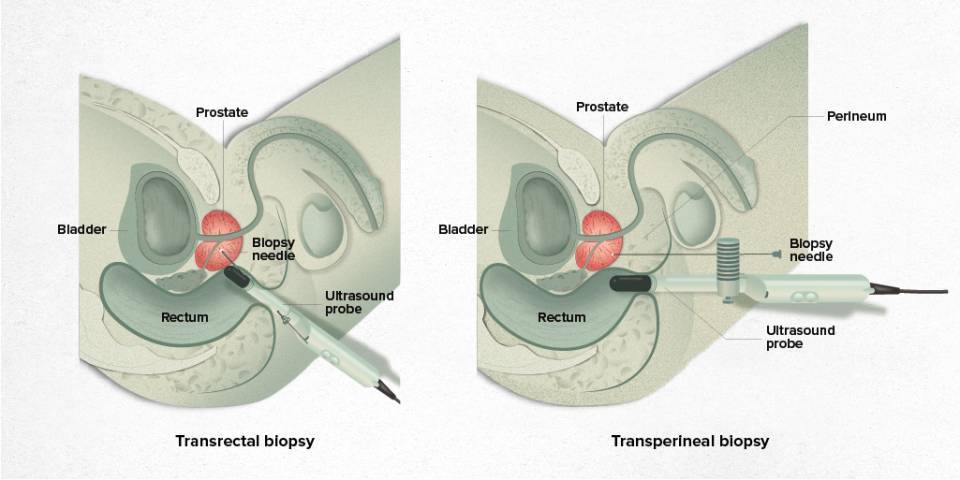
Sampling can be done transrectally (through the rectum) or transperineally (through the perineum or pelvic floor). The transrectal route can be performed under local anaesthesia, but the transperineal route usually requires anaesthesia or sedation, although in some cases it can be done under local anaesthesia.
In both cases, apart from targeted biopsies in suspicious areas, systematic biopsies of the entire prostate are obtained. The extracted tissue is analysed later by the Pathological Anatomy Unit.
Why is it recommended?
MRI-ultrasound fusion biopsies are recommended in patients who have an earlier MRI of the prostate that shows indeterminate or suspicious lesions.
It is also performed on patients diagnosed with prostate cancer who are following an active surveillance protocol. This protocol consists of monitoring very low-risk tumours in patients who meet a series of criteria. These patients are periodically checked with laboratory tests, MRI and biopsies.
How is it performed?
The biopsy is done via ultrasound and the prostate is sampled using a sampling needle (Tru-Cut). It can be performed transrectally or transperineally.
To perform the ultrasound correctly and take the samples while minimising the risk of infection, the rectum must be prepared and preventive antibiotics (prophylaxis) taken.
There are several guidelines for antibiotic prophylaxis, taking into account the patient's possible drug allergies. In all cases, the antibiotic regimen must be started the day before the biopsy. The regimen is usually completed with a second dose on the same day as the biopsy in the afternoon. However, depending on the type of antibiotic that has been used, it may also have to be taken a few days after the test.
The rectum is cleaned via an enema the night before the biopsy.
If the biopsy is performed under local anaesthesia (transrectal route), fasting is not necessary and the patient can eat before the biopsy.
If the biopsy is performed under sedation (transperineal route), the patient must undergo an anaesthetic procedure and will therefore have to fast for 6 hours before the test.
Will I be able to take my medication?
A biopsy is a surgical procedure to take multiple samples of prostate tissue using a sampling needle, so there is an inherent risk of bleeding.
Therefore, anticoagulant treatments (e.g. Sintrom, Heparin and new generation anticoagulants) and antiaggregates (e.g. aspirin and clopidogrel), which increase the risk of bleeding, usually have to be stopped a few days before the procedure.
Other medication, however, with these exceptions, can be taken on the day of the biopsy. In any case, the doctor who indicates the biopsy will explain what to do with your usual medication. The medical team contacts patients a few days before to remind them about the preparation for the test and to clarify any doubts they may have.
What happens during the test?
Before starting the test, the prostate MRI images are incorporated into the ultrasound software to be able to superimpose the resonance and ultrasound images.
If the biopsy is to be done under sedation, this is started after the digital rectal examination.
If the biopsy is to be performed under local anaesthesia, first the digital rectal examination is done and the transrectal ultrasound introduced, followed by the anaesthetic injection.
In both cases, the prostate ultrasound is performed using the transrectal transducer. Ultrasound images are obtained to be superimposed with the MRI images to be able to make the 3-D model, which facilitates taking a biopsy of suspicious areas.
Once the NMR-ultrasound images have been fused, the prostate samples are collected using the sampling needle. The needle samples are taken transrectally (through the rectum) or transperineally (through the perineum or pelvic floor), depending on the case.
The samples are sent to the Pathological Anatomy laboratory for analysis.
How long does it take?
The test usually takes less than an hour and is done on an outpatient basis. Thus, the patient is in hospital for about an hour or two.
If the biopsy is taken under sedation, a brief period of resuscitation is required after the anaesthesia, usually lasting less than an hour.
What happens after the test?
After the procedure, you should rest for a few days and avoid overexertion in any exercise or movements you make. You should also drink plenty of water after the test.
24 hours after the test, you will be ready to return to an almost normal life, avoiding all sports and especially not putting pressure on the perineum or pelvic floor. You should not ride a bike or motorbike for 2-3 weeks after the biopsy is performed.
Blood in the urine or stool is normal in the first few hours after the biopsy, and this may continue for a few days. It is also normal to have blood in your semen for weeks after the procedure. Discomfort or pain is usually mild and can be eased with paracetamol or ibuprofen.
What are potential complications?
Any significant bleeding, with clots, from the urethra or rectum should alert the patient. If the bleeding does not improve, you should go to emergency services.
Occasionally, urinary retention occurs that requires the placement of a bladder catheter for a few days.
Before the test you have to take antibiotics to prevent infection. If you develop a fever a few days after the test, despite the antibiotics, you should go to the emergency department to assess the need for more antibiotics.
Content related
Substantiated information by:


Published: 19 October 2022
Updated: 19 October 2022
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox