What is an Electroencephalogram (EEG)?
Electroencephalogram (EEG) is a test that evaluates the electrical activity of nerve cells (neurons) in the cerebral cortex (the nerve tissue that lines the brain). It is a neurophysiological test that detects and measures the function of neurons from an electrical point of view, using electrodes that are placed on the person's scalp.
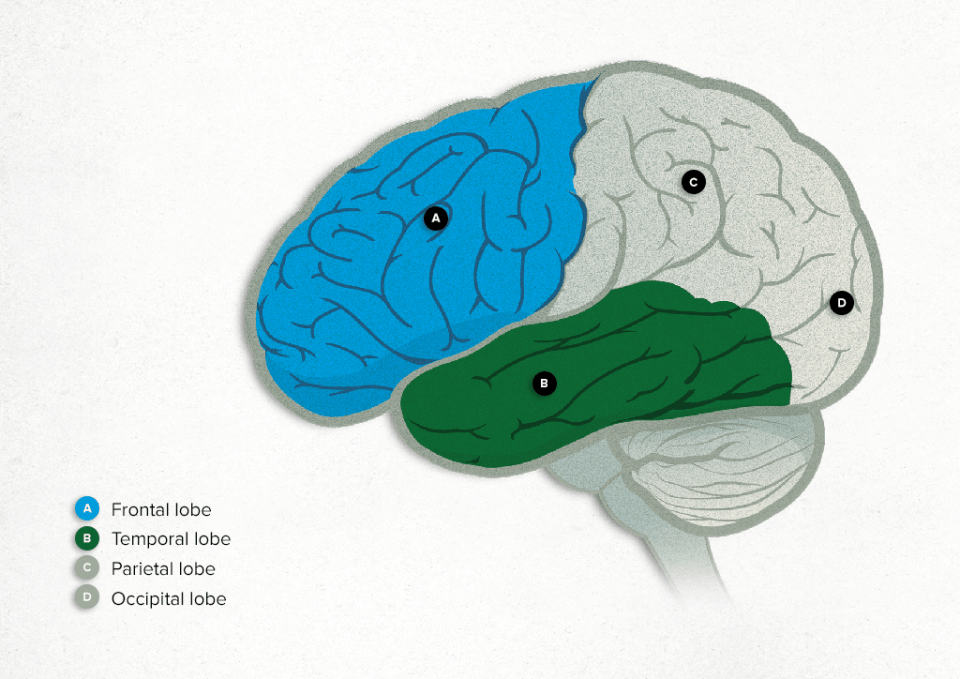
This test means the brain activity of neurons in the two cerebral hemispheres and their four lobes (frontal, temporal, parietal and occipital) can be detected. It cannot detect the activity of neurons in the cerebellum, the brainstem, or the deep areas of the brain. Brain cells communicate through electrical impulses and are always active, no matter whether the person is awake or asleep.
Electrical activity in the brain is seen in the form of waves of different frequency (the main ones, from fastest to slowest, being beta, alpha, theta and delta) and amplitude (low, moderate or high). These vary depending on the area of the cerebral cortex and the status of the person (whether awake or asleep, or whether or not they have a brain injury or epilepsy).
Why is recommended for?
An electroencephalogram (EEG) is one of the main tests used to diagnose epilepsy. In patients with epilepsy, the EEG often detects abnormal waves (known as epileptiform waves) that stand out from normal brain activity. An EEG helps to determine whether the epilepsy is generalised; whether the epileptiform waves affect both hemispheres at the same time; or whether it is more focal with abnormal waves localised in a specific part of the cerebral cortex.
In addition to being used for diagnosis, this test can be used for clinical follow-up or for the withdrawal or introduction of anti-epileptic medication in patients with epilepsy.
Other uses of EEG in epilepsy are:
- Detecting a non-convulsive epileptic status.
- Diagnosing specific epileptic syndromes, such as absences, Lennox-Gastaut syndrome (a type of childhood epilepsy), West syndrome (an epileptic encephalopathy that begins in the first year of life) and Rolandic epilepsy (a type of childhood, focal epilepsy).
- Identifying pseudoseizures, which are attacks that may seem like epileptic seizures, but are not and have a functional origin.
An EEG is also a useful test for other situations, such as:
- Patients with a reduced level of consciousness or in a coma, especially when the origin is unknown.
- Encephalopathies of any origin (metabolic, infectious, toxic).
- Herpes encephalitis: serious viral infection of the central nervous system
- Creutzfeldt-Jakob disease: a degenerative disorder that progresses rapidly and causes dementia.
- Cerebral hypoxia or lack of oxygen to the brain.
- Confirming brain death, when the EEG shows no electrical activity in the brain (or is “flat”).
- Studying sleep and its disorders (e.g., sleepwalking, excessive daytime sleepiness and narcolepsy).
What preparations are needed?
In the days leading up to the test, the patient should:

Take their usual medication, without changing the frequency or dosage (this is especially important in the case of anti-epileptic drugs).

Maintain a regular schedule.

Avoid introducing new medicines.

Avoid using drugs.

Avoid consuming excess alcohol.

Avoid caffeine intake.

Wash their hair the night before the day of the study. The patient should not use hairspray or gel. These hair products can make it difficult for the electrodes to adhere to the scalp properly, causing them to fall off during the test.

Occasionally, the doctor will ask for the EEG to be done after a day's sleep deprivation. This means that the patient should not sleep the night before the test. In these cases, the test is performed first thing in the morning.
How it is performed?
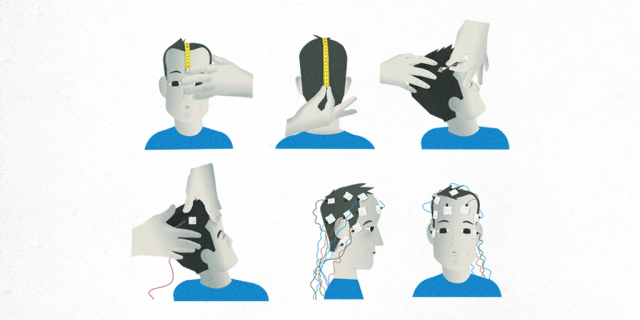
To perform an electroencephalogram (EEG), the proper equipment and a skilled technician are required.
The equipment consists of:
- A tape measure
- Thick-tipped marking pens
- Cotton swabs
- Surface electrodes
- Scalp cleansing paste
- Conductive paste (which fixes the electrode onto the scalp and helps in recording the brain's electrical activity)
- Gauze
- Input box for a signal amplifier
- Digital acquisition and record review device
The electrodes should be positioned so as to allow electrical activity to be recorded efficiently, and with minimum distortion. They are placed on the scalp so as not to cause pain or become displaced throughout the entire test. Their positioning should cover all regions of the cerebral cortex and the midline. 21 electrodes are put in place, and each one is given a name (frontopolar, frontal, central, parietal and occipital) and a location (left, right, midline).
Positioning takes 30 minutes to ensure that the electrodes are placed correctly and symmetrically on the anatomical areas. An electrode is placed on each earlobe and to the sides of the eyes. This allows an electrooculogram to be carried out, to assess eye movements, which often alter the electroencephalographic recording. It is very useful for the EEG recording to be synchronised with a video recording, to see possible epileptic seizures or normal movements.
The EEG is recorded for a minimum of 30 minutes and the patient is usually lying on a bed or sitting comfortably on a couch. In some specific cases, it may be longer; for example, 1 hour if there has been sleep deprivation the previous night. They are asked to open and close their eyes and take quick deep breaths for 3 minutes. At the beginning or end of the test, a high-intensity light is placed in front of the patient and flashed at different frequencies above the eyes when closed.
Will I be able to take my medication?
Yes. The test should be performed under the patient's typical conditions, so that it is representative of what has been happening to the patient recently. This is why the patient should continue taking their usual medicines (the same number of pills at the same times), especially those used for epilepsy.
What happens during the test?
Before the test, the technician will measure the patient's head and mark specific points on the surface of the scalp with a special thick-tipped pencil to indicate where the electrodes should be placed. They will also apply gel to the scalp to place the electrodes, as well as a conductive paste, to ensure that they adhere correctly, and to improve the quality of the recording.
During the test, the electrodes are connected to the input box that amplifies the brainwave signal using conductor cables, and the recording is made on a computer.
The patient is invited to relax and close their eyes in a comfortable position, on a bed or armchair. The technician will ask them to open and close their eyes at different points. They will be asked to breathe quickly and deeply for 3 minutes.
A light will be placed in front of the patient's eyes. This light emits intermittent bursts at different frequencies for 2 minutes, and they will be asked to open their eyes between bursts. If the patient was deprived of sleep the night before, the intensity of the light in the room will be reduced and the patient will be invited to relax and fall asleep in bed.
In special situations, depending on the patient’s characteristics and the recording, they might be asked to perform some simple calculations, read a paragraph, look at a fixed image or open and close their hand.
The whole test is supervised by a technician who will be responsible for the quality of the recording and will take note of any incident. The patient is asked to notify the technician if they experience any abnormality during the recording.
How long does it take?
A conventional electroencephalogram (EEG) recording takes about 30 minutes, and preparing the patient for the test also takes about 30 minutes (so total duration is about 1 hour).
A sleep-deprived EEG recording lasts 60 minutes (i.e., a total of about 90 minutes including 30 minutes to set it up). It consists of two parts. The first part (30 minutes) is the same as a conventional EEG. In the second part (30 minutes), the room light is dimmed and the patient is encouraged to sleep for 30 minutes. In these cases, intermittent light stimulation can be performed at the end of the recording.
The EEG recording for the diagnosis of brain death should last 30 minutes. It involves intermittent light stimulation on two occasions and the application of painful stimuli to the patient to confirm that the recording does not change.
In special situations, the doctor may request an EEG recording of several hours or even days (EEG monitoring). In these cases, a solution is applied to the scalp to prevent the electrodes from coming loose.
What happens after the electroencephalogram (EEG)?
At the end of the test, the technician carefully removes the electrodes with gauze and alcohol, in order to not damage the patient's scalp. During this period of time, which usually lasts 5-10 minutes, the technician will ask the patient if they noticed anything abnormal during the test. The patient can then leave the hospital.
The recording is stored digitally, and will be reviewed by a doctor who will produce a report. The report should include the patient's name, age and sex, the medication they take, the reason for the consultation, the date of the test, and the test report. The technical conditions, the results, their interpretation, and the conclusions should all appear in this report. The EEG report is sent to the doctor who requested the test, and the most appropriate action will be taken in the context of the individual patient, in accordance with the results.
What are the possible complications?
Electroencephalogram is a safe test that has been used for more than 100 years. During an EEG, the electrodes do not transmit any sensation, nor do they cause pain or emit discharges. They only record the brain waves. The adhesive gel and the conductive paste do not cause any alterations or allergies. If the electrodes have not been placed delicately enough, it is possible that they may cause slight irritation on the scalp, which will disappear after a few hours.
Special situations
The electroencephalogram (EEG) can detect epileptic activity. Therefore, provocation techniques are performed during the test, such as hyperventilation for three minutes, intermittent light stimulation and sleep onset after sleep deprivation the previous night. These operations facilitate the detection of epileptiform activity.
However, these techniques also have a very low risk of causing epileptic seizures. If the patient has convulsions or loses consciousness during the test, the technician presses an alarm button to summon a doctor immediately.
The first thing that should be done in the event of an epileptic seizure, is to remain calm and act professionally, as the patient usually fully recovers within minutes after the seizure. Objects that could hit the patient should be removed, and tight clothing (belt, shirt collar, tie) should be loosened. No objects should be placed between the teeth. When the seizure has stopped, the patient should be placed on his side to prevent any remaining vomit in the mouth from passing into the respiratory system. It is also important to ensure the mouth and airways are clear. What happens during a seizure should be observed (e.g. head deviation or sequence of movements).
During EEGs, the patient is routinely videotaped so the features of any seizure that occurs can be subsequently reviewed and correlated with the simultaneous EEG recording.
Related contents
Substantiated information by:


Published: 27 April 2022
Updated: 20 March 2025
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox