What is a Colonoscopy?
A colonoscopy is a safe and effective test to examine the inside of the large intestine, including the rectum. It is used to evaluate symptoms such as digestive bleeding, chronic diarrhoea or changes in bowel habits. It is also a key tool in the prevention and early detection of colorectal cancer.
How is a Colonoscopy done?
It is performed with a colonoscope, a flexible tube with a camera at the tip to obtain detailed images of the intestine. In addition, it has a special channel for inserting instruments and performing treatments, such as removing polyps or taking biopsies.
How to prepare for a Colonoscopy?
The colon has to be completely clean for the examination to be effective. The preparation begins the day before the test, following a fibre-free diet. Then, a laxative has to be taken; this is a special solution to clean out the intestine. The medical team provide precise instructions on how and when to take this solution. The preparation must be completed and nothing must be drunk at least six hours before the procedure in preparation for anaesthesia. It is advisable to have someone with you during administration of sedation or anaesthesia.
It is a very easy, straightforward test. Moreover, there is no stress and it doesn't cause any discomfort.

Can I take my medication?
Most medications can be taken as usual, but some may interfere with the preparation or the examination. The healthcare team should be informed about the medication you are taking, particularly aspirin-derived products, anti-inflammatory drugs, anticoagulants (warfarin, dabigatran, apixaban or heparin), clopidogrel or other antiplatelet drugs, insulin, obesity medication or iron supplements. You should also inform the team of any allergies to medications and whether you have an implantable cardioverter defibrillator (ICD) or other medical device.
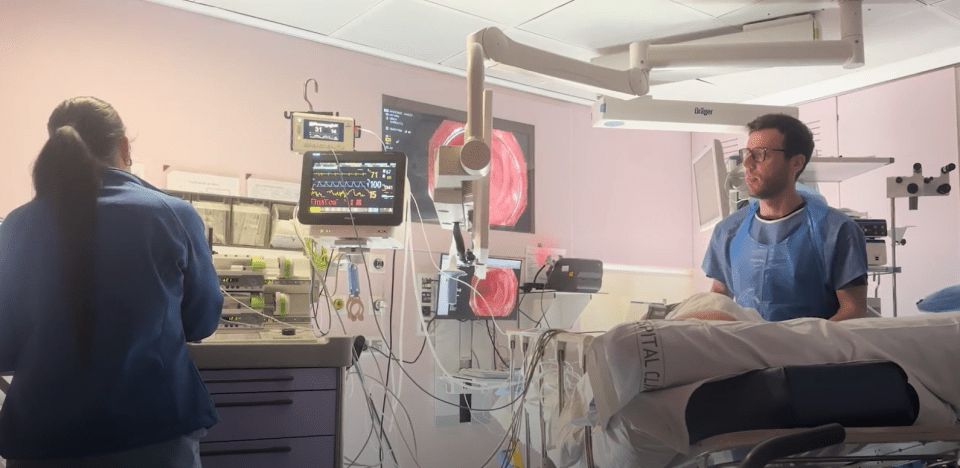
What happens during a Colonoscopy?
The patient must be naked from the waist down and placed on one side or facing upwards on a trolley. In order to visualise the mucosa well, the doctor may introduce gas (air or CO2) into the bowel. In the majority of cases, a rapid elimination general anaesthetic is administered, since the distension of the bowel walls and the advance of the colonoscope, through certain curves or difficult points, can cause abdominal discomfort. A catheter is inserted in a vein of the hand or arm, as well as some electrodes to monitor vital signs.
You will not feel pain during the test. The health professional will slowly advance the colonoscope through the large intestine until it reaches the area that connects the small and large intestine (cecum). Occasionally, the patient is asked to change position (from the side or facing upwards) in order to apply gentle pressure on the abdomen and help the progression of the colonoscope.
As the colonoscope is slowly withdrawn, the bowel lining is examined again. On those occasions when the colonoscope is unable to pass through the entire intestine, an additional test has to be performed.
How long does a Colonoscopy last?
The procedure generally lasts less than 45 minutes. If the preparation and recovery are taken into account, it lasts between two and three hours.
What happens if the Colonoscopy shows something abnormal?
In the cases in which an additional evaluation is needed, an instrument is passed through the colonoscope in order to obtain a biopsy (a small specimen of the bowel lining). Biopsies are used to identify many conditions, and are often performed despite there is no suspicion of cancer.
When a colonoscope is performed to identify bleeding sites, drugs are injected through the colonoscope or the bleeding vessels are sealed with thermal treatment (cauterisation) or by using small clips.
Polyps can be found during the examination, and it is very possible that they are removed during it.
At first you receive a bit of psycological preparation for what you will have. They insert a tube with a light in your anus, then they look around inside and directly remove any polyps they find.

What happens after a Colonoscopy?
The patient remains under observation until most of the effects of the sedatives or anaesthetics have worn off. For this reason, it is advisable to be accompanied during and after the examination.
It is possible to have cramp or swelling due to the CO2 introduced into the bowel during the examination. These effects usually disappear rapidly when the gas is expelled.
In general, you can eat after the colonoscopy, although in cases in which polyps have been removed (polypectomy), you should follow a special diet and restrict some activities.
It is also normal to have small losses of blood for several days after the procedure.
The health team will explain the test results. Normally, you have to wait a certain time to obtain the results of the biopsies.
What are the possible complications of the Colonoscopy?
The colonoscopy and the polypectomy are generally safe. A possible complication that could arise is a perforation or a tear of the intestinal wall that could require surgery. You could also bleed in the area where the biopsy was performed or where the polyp was removed, although it is mild. The bleeding can stop by itself or be controlled through the colonoscope. It rarely requires follow-up treatment. Some patients may have a reaction to the sedatives, or a complication of a heart or lung disease.
Although the complications after the colonoscopy are rare, it is important to recognise the early signs of any complications. In this sense, it is advisable to contact the medical team if you note intense abdominal pain, fever and shivering, or continuous rectal bleeding.
Related contents
Substantiated information by:

Published: 6 June 2018
Updated: 11 March 2025
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox