Treatment of Glaucoma
Glaucoma is a chronic disease because it involves damage to the optic nerve that cannot be regenerated. The aim of treatment, therefore, is to slow the evolution of the condition and lower the intraocular pressure, even in patients with normal pressure at the time of diagnosis.
The therapeutic options are eye drops, treatment or laser surgery. It is important that the patient and health care professional work together to ensure the treatment is effective.

Diet. A balanced diet rich in vitamins and antioxidants (particularly green leafy vegetables) can help prevent damage to optic nerve fibres.

Exercise and sun. Patients should protect their eyes from the sun, do moderate exercise and maintain a healthy weight.

Vitamin supplements. There is some evidence that ginkgo biloba, magnesium and citicoline can reduce damage to optic nerve fibres. They should be used under medical supervision because high doses can have side effects such as increased bleeding, for example.

Medications in the form of eye drops. In most patients, glaucoma is controlled with eye drops applied on a daily basis in order to reduce the intraocular pressure. Some eye drops reduce the amount of fluid produced within the eye, while others decrease the pressure by increasing the amount of fluid that drains from the eye.
There is no specific pressure that is perfect for all patients. The target pressure sought with the eye drops depends on the patient’s degree of glaucoma and intraocular pressure at the time of diagnosis. The ideal pressure for each patient must be individualised to a value that ensures they do not suffer further vision loss.
The application of eye drops varies depending on the medication used. Some eye drops are applied once a day and others two or three times a day. Some patients need to receive treatment involving more than one medication to control the intraocular pressure.
Patients must be aware that they have to follow the treatment closely and apply the drops consistently every day to prevent the disease from worsening. It is therefore very important that they trust in their glaucoma specialist.
Eye drop treatments for glaucoma can cause some side effects that range from mild to severe. The most common side effects are:
- A burning sensation in the eye.
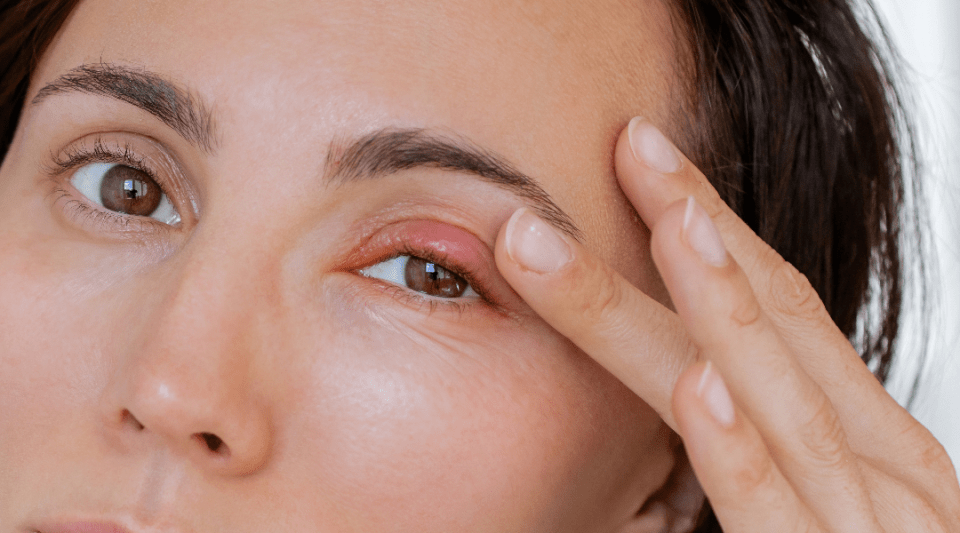
- Reddening of the eye or the area around the eye.
- Changes in heart rate (pulse).
- Changes in overall energy levels (feeling more tired).
- Changes in breathing (especially in patients with asthma or bronchitis).
- Dry mouth.
- Blurred vision.
- Growth of eyelashes.
- Changes in the colour of the eyes and the skin around the eyes.
If you notice any side effects to the treatment, you should discuss them with your doctor before you stop using the eye drops.
Laser treatment is usually a second-line option and helps improve the eye’s drainage system. These procedures are normally carried out in an ophthalmology clinic and patients can return to their routine habits later that day. There are two main types of laser used to treat glaucoma.

Trabeculoplasty. This laser technique is for patients with open-angle glaucoma. Laser energy is applied to the filtration angle to improve the drainage system, thus allowing the intraocular fluid to exit the eye more easily and reduce the pressure.

Iridotomy. This type of laser treatment is used for angle-closure glaucoma. A small incision is made in the iris (the coloured part of the eye) to improve the drainage of aqueous humour. The technique increases the space at the front of the eye and reduces the possibility of a sudden increase in intraocular pressure.
When drug therapy is not enough to reduce intraocular pressure, some patients require a surgical intervention. Glaucoma surgery does not improve the patient’s vision, as a damaged optic nerve cannot be regenerated, but it does serve to reduce the intraocular pressure to appropriate levels required to maintain vision.
The most frequent procedures are:

Filtering surgery. The procedures used most often are trabeculectomy and non-perforating deep sclerectomy. A small flap is cut in the sclera (white of the eye) through which another channel is created to allow the aqueous humour to drain from the eye. A pocket is made in the conjunctiva (a membrane covering the surface of the eyeball) where the fluid will accumulate (filtering bleb) and remain safeguarded under the eyelid and therefore out of sight. In the bleb, the fluid from the eye is absorbed into the surrounding tissues, thus reducing the pressure.

Drainage systems. A drainage tube is inserted into the eye and directs the fluid to a more spacious area called a reservoir. This is situated under the conjunctiva (membrane covering the surface of the eyeball) and the sclera (white of the eye). The fluid is then absorbed by the surrounding veins.
Glaucoma surgery requires postoperative care and regular follow-up appointments for a few months to achieve the desired outcome. The postoperative treatment often includes the administration of anti-inflammatories and use of antiscarring techniques to prevent the newly created filtration system from closing or providing too much drainage.
Just because a patient undergoes surgery it does not mean they are cured, they must attend regular check-ups to ensure the disease does not progress further.
- Minimally invasive glaucoma surgery. New glaucoma micro-implants applied with minuscule incisions have been developed in recent years which allow the patient to recover more quickly and with fewer complications. These implants are inserted directly in the transparent section of the eye and an applicator is placed in the drainage system. At the present time, this technique is reserved for patients with mild to moderate glaucoma.
- Sustained-release systems. There are some sustained-release medications that can be administered to patients in the clinic every 3–4 months. This treatment is still being researched, but it is quite well developed.
Substantiated information by:



Published: 19 October 2018
Updated: 19 October 2018
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox
Glaucoma related news
30 November 2023
What are the most common eyelid diseases?
16 October 2023