Breast Cancer treatment
Once the breast cancer has been diagnosed, a multidisciplinary team evaluates each case on an individual basis so they may decide upon the most appropriate treatment.
The team comprises all of the healthcare professionals directly involved in the diagnostic and therapeutic process, such as gynaecological surgeons, radiologists, nuclear medicine specialists, pathologists, radiotherapists, oncologists, plastic surgeons, and oncological and surgical nursing staff.
Once the team reaches a collective decision, the specialist will inform the patient about their choice and explain the treatment. In the past, early-stage breast cancer treatment initially commenced with surgery followed by chemotherapy (systemic treatment) and radiotherapy (adjuvant treatment). Nowadays, chemotherapy may be started before surgery and radiotherapy. Thanks to this strategy, in certain cases conservative surgery can be implemented which would otherwise be unfeasible.
In advanced stages, the primary treatment is chemotherapy, although surgery or radiotherapy may be used in specific situations.
To select the best treatment, the doctors need to know the type of cells that form the tumour and type of receptors.
- Type of cells. What are healthy cells like? Healthy cells have receptors that are stimulated by substances entering the cell from the blood supply and which consequently promote correct growth. Tumour cells can use these receptors to accelerate their growth. If tumour cells preserve these receptors, i.e., they did not lose them when they transformed into tumour cells, then the treatment can take advantage of them. But how? By directing drugs which act as these receptors.
- Type of receptors. Breast cancer treatment is currently directed towards the following types of receptor:

Hormone receptors
Hormone receptors detect the blood levels of female hormones, oestrogens and progesterone, throughout the lifetime of all women. Therefore, when a girl reaches adolescence and her blood oestrogen levels increase it causes her breasts to grow, along with all the other bodily changes associated with puberty. On the other hand, the decline in blood oestrogen levels during the menopause leads to breast atrophy (wasting).
Hormonal therapy can be used on any tumours that conserve these receptors. The treatment is usually based on tablets that block the cancer cells’ hormone receptors and therefore prevent oestrogens from stimulating the growth of malignant cells.

HER2 receptor. HER2 is a protein involved in cell growth. It is only overexpressed in 1 in every 5 breast tumours. If the tumour cells have a lot of HER2 receptors, compared to what is usually observed in a normal cell, then these malignant cells will grow much more quickly than others. Anti-HER2 treatments block this receptor and impede further tumour growth.
Dr. Aleix Prat, a breast cancer oncologist at Hospital Clínic, answers frequently asked questions about breast cancer.
There are different therapeutic approaches to treating breast cancer: surgical treatment and non-surgical treatment.
The choice of one or a combination of treatments is based on how much the disease has spread. Nevertheless, the final treatment choice varies between individual patients depending on their overall health and underlying illnesses.

Breast surgery. The objective is to eliminate the tumour and discover whether or not the axillary lymph nodes have been affected by the cancer. Based on the results, the surgeon will remove more or less lymph nodes. Surgery may be:
- Radical. The whole breast is removed (mastectomy).
- Conservative. The tumour plus a safety margin are removed and the rest of the breast is preserved, so long as it produces an aesthetically acceptable result.
The choice between radical and conservative surgery depends on tumour size, breast size and the patient's wishes. There may be other determining factors that the surgeon and oncologist must evaluate before taking their decision.

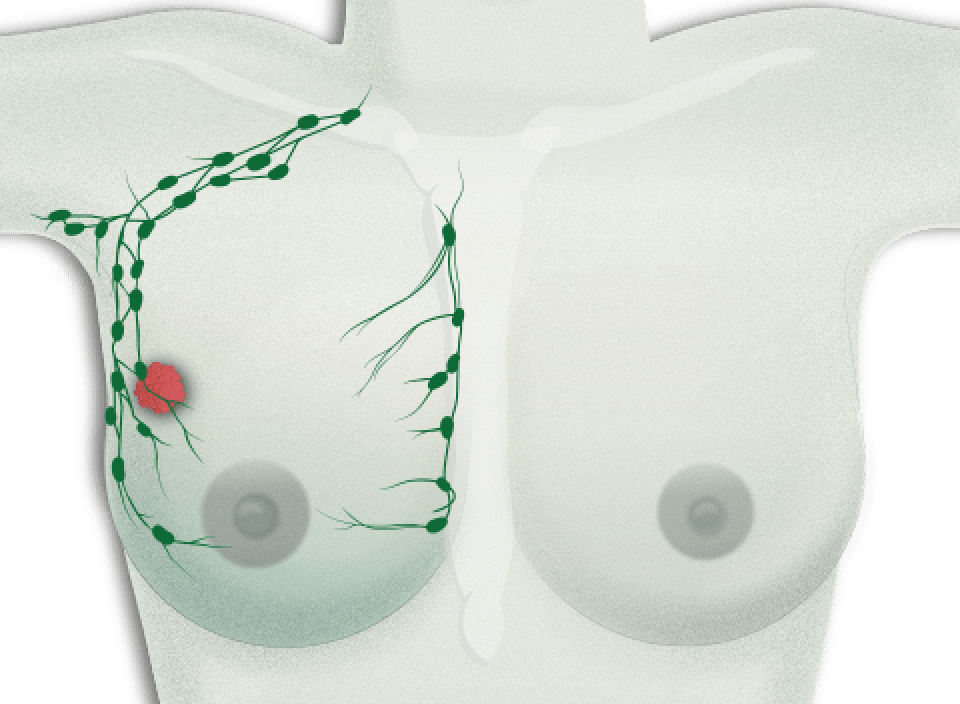
Axillary lymph node surgery. Surgery on the lymph nodes found in the armpit depends on whether or not they are affected by the tumour.
- Lymph nodes are affected.The surgeon will perform a more radical operation in the axillary area to eliminate all of the cancer. Recent studies have advised against a complete lymph node dissection if only a small number of nodes are affected and the patient's overall condition permits partial dissection. One of the most troublesome side effects of axillary lymph node dissection is lymphoedema in the arm. This condition manifests with swelling in the arm because of poor lymph circulation after removing a large number of axillary lymph nodes.
- No lymph nodes are affected. Only the first few lymph nodes in the chain are removed, what are known as the sentinel lymph nodes. This helps to reduce lymphoedema in the arm.
During the operation in which the tumour is removed, the surgeon will also take out some axillary lymph nodes. This is done in order to discover whether or not the cancer cells have spread to the lymph nodes. Whenever breast cancer is detected in later stages, then there is a greater possibility that cancer cells will have spread to the axillary lymph nodes. However, this is not always true, as some more aggressive tumours invade the lymph nodes at a much earlier stage. Recent clinical studies have shown that when only a few sentinel lymph nodes are affected then they do not always need to be resected. Regardless of this, each patient requires a different treatment plan.
Depending on the cancer’s degree of extension, only the first lymph node in the chain (the sentinel lymph node) will be removed. The likelihood of the tumour cells forming micro-metastases in other organs increases whenever a greater number and larger lymph nodes are affected by the cancer.
The armpit contains three levels of lymph nodes, from those closest to the chest, up to the ones found near the collarbone. In principle, lymph node dissection aims to remove just the first two levels of axillary lymph nodes, even in cases where they are affected by the cancer, in order to reduce the risk of lymphoedema, i.e., inflammation in the arm.
Although the technique of dissecting just the sentinel lymph nodes has produced a significant decrease in morbidity and improved quality of life for patients, often the axillary lymph nodes need to be removed completely (a lymphadenectomy) which can lead to chronic lymphoedema and back pain, thus reducing the quality of life.

Radiotherapy. Radiotherapy, along with surgery, is a local treatment whose objective is to eliminate any small remnants of tumour in chest or axillary areas. Microscopic tumour cells may still be present after surgery; these are invisible to the human eye and cannot even be detected by a mammogram or MRI scan. Radiotherapy also sometimes needs to be performed in the supraclavicular area, that is, the space found between the shoulders and the nape of the neck.

Chemotherapy. Chemotherapy is a type of treatment that destroys any fast-growing cells. It attacks cells when they are dividing and reproducing. The quicker the cells grow, then the quicker they divide and hence chemotherapy is even more effective.

Hormonal therapy. It is the first treatment to target the hormone receptors. Hormonal therapy is indicated for patients with tumours that possess hormone receptors, i.e., hormone receptor-positive tumours. The tumour is said to express positive hormone receptors if more than 1% of the tumour cells feature the receptors. Hormonal therapy is normally administered as tablets and the treatment tends to last for five years.
The most important drugs are:
- Tamoxifen. This drug can be beneficial for both younger women, who still menstruate, and post-menopausal patients.
- Aromatase inhibitors. These are only indicated for post-menopausal women.

Anti-HER2 treatment. The aim of this treatment is to block the HER2 receptor. The HER2 receptor is located on the surface of tumour cells in one in five breast cancers. If the tumour has an excessive amount of these receptors then it is called a HER2-positive breast cancer. When the receptor is blocked by administering anti-HER2 drugs, such as trastuzumab or lapatinib, then the carcinoma cells suffer significant damage and can even experience cell death. It is a very effective treatment and has been shown to reduce the number of recurrences by almost 50%.
Before starting treatment, or after the first dose of chemotherapy, a central venous catheter (CVC) needs to be inserted to simplify the administration of medicines and to avoid damaging peripheral veins. CVCs are inserted in an operating room using local anaesthetic; the procedure does not require an overnight stay.
You must wear this catheter throughout the treatment. Your oncologist and doctor will decide when it should be removed by taking into account the initial diagnosis and prognostic factors at the start of treatment, which could mean you need to wear the device for up to 12 months.
The catheter should be checked 3 months after completing chemotherapy and the last administration of chemotherapy drugs. This check-up should be repeated every 3 months after finishing the treatment. If a PICC type central catheter is inserted, then it can be removed on the same day as the last dose of chemotherapy.
Existen diferentes efectos secundarios al tratamiento que dependen del tipo específico de la quimioterapia administrada. Es muy importante que el médico informe sobre ellos antes del inicio del tratamiento.
Entre los síntomas que pueden aparecer se encuentra: cansancio (astenia), cambio en el gusto de los alimentos, náuseas, vómitos, caída de pelo, inflamación de la mucosa de la boca, fiebre, estreñimiento/diarrea, dolor abdominal y muscular, urticaria y lesiones en las uñas. Ante cualquier duda, es recomendable consultar con el médico.
La radioterapia puede estar asociada a una irritación cutánea, inflamación de la mucosa esofágica (esofagitis - dificultad para tragar), cansancio y neumonitis o inflamación del tejido pulmonar, que suelen aparecer meses después de haber completado el tratamiento.
Different breast reconstruction techniques are practised and this depends on whether or not the breast can be preserved.

In cases where the breast is preserved, surgeons use aesthetic improvement techniques that do not require a prosthetic implant but rather they take fat deposits from the patient (thighs, abdomen, back or legs) and use them to correct small volume defects after removing the tumour.

In cases where the entire breast is removed, the simplest reconstruction method is a silicone breast implant. First of all the surgeon will insert a temporary implant called a tissue expander, a balloon-like structure that is gradually inflated to stretch the skin. Later they will replace it with a permanent implant or the patient's own tissue. Silicone is a material used in several medical devices inserted inside the body, such as pacemakers, valves, catheters, and more; its safe use in breast reconstruction has been demonstrated beyond doubt.

To achieve an even better final result, sometimes the healthy breast also needs to undergo treatment in order to elevate it or decrease its volume so that both breasts look alike.

Three or four months after breast reconstruction, you will undergo reconstruction of the areola and nipple using a very straightforward technique performed under local anaesthetic and which does not require a hospital stay.
It is important to bear in mind that breast reconstruction does not complicate future check-ups.
Acute complications of reconstruction are surgical wound infection, infection of the synthetic material or muscle used for the implant and suture dehiscence (the two borders of the wound split open). In the long term you may experience pain in the area from where the muscle was extracted, limited mobility or problems (rejection) with the supporting mesh.
Reconstruction will not hinder physical examinations, radiological imaging tests or patient follow-ups in general. In some cases where a partial implant has been inserted it could complicate taking a mammogram and so medical resonance imaging (MRI) is used.
Substantiated information by:




Published: 20 February 2018
Updated: 20 February 2018
Subscribe
Receive the latest updates related to this content.
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox