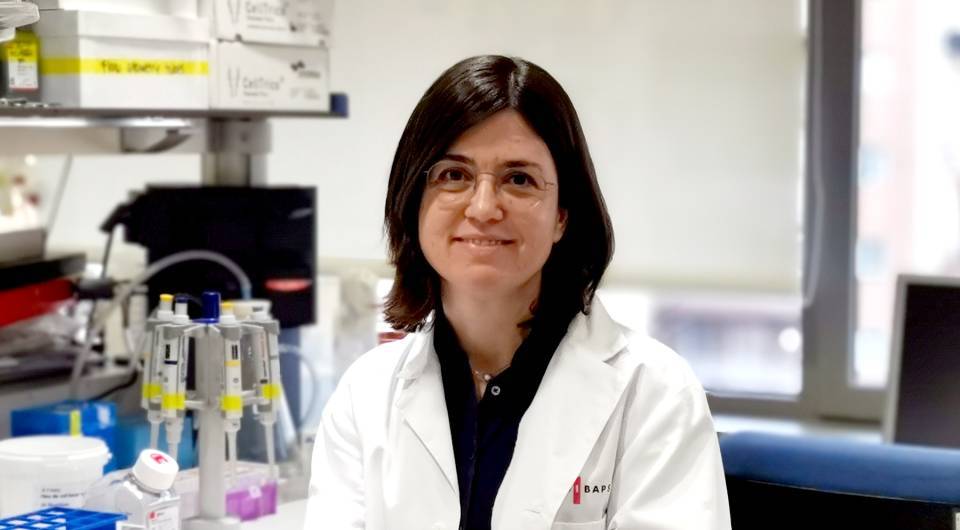
Inflammatory bowel disease is a term that covers different chronic inflammatory disorders of the digestive system, including Crohn disease and ulcerative colitis. Both disorders can affect people of any age, although most patients are diagnosed in the second or third decade of life. “There is a peak of incidence around 60 years, but most diagnoses are in young people”, explains Azucena Salas, head of the IDIBAPS group on Inflammatory bowel disease, which is also part of CIBERehd.
Ulcerative colitis and Crohn disease share similarities, but they also have many differences, such as the region of the digestive system in which they are located. Thus, while the former affects the colon and rectum, the latter may affect any area of the digestive tract. “Tissue analysis and imaging tests show that the lesions associated with these disorders may also be different. For example, perianal fistulas and fistulas of the gut are characteristic of Crohn disease and do not appear in colitis”, indicates Salas. “In general, Crohn disease is more heterogenous than ulcerative colitis, with highly diverse manifestations and symptoms. It is precisely this heterogeneity that generates much interest among researchers, who devote considerable effort to understanding what is happening”.
The most common symptoms of Crohn disease are diarrhea, abnormal intestinal transit, and abdominal pain. In ulcerative colitis, the most common symptoms include diarrhea, stools with mucus and/or blood (rectorrhagia), numerous small stools, or a frequent desire to evacuate the bowels, and an urgent need to defecate.
Both Crohn disease and ulcerative colitis are complex disorders, as there are many mechanisms involved in their development and progression. Moreover, their etiology; that is, the factor that causes them, is still unknown. Research focuses principally on the prevention and cure of these diseases. With this goal in mind, researchers are studying the genetics of the patients, the influence of the environment, and the role of the intestinal microbiota in modulating the immune system and the inflammatory reaction.
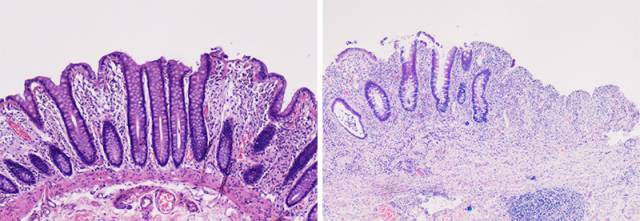
Hematoxylin-eosin staining of healthy intestinal tissue (left) and intestinal tissue affected by ulcerative colitis (right).
Goal: to cure the disease
Identifying biomarkers for diagnosis but also for risk and for predicting response to treatment is another of the main areas of research in Crohn disease and ulcerative colitis. “There are currently no markers that allow us to see where the disease will go. Whether it will be severe or mild. Whether more or less aggressive therapy will be required. This makes it difficult to choose the best treatment for each patient”, says the researcher. “In terms of therapeutic strategies, we have effective drugs, such as corticosteroids and anti-inflammatory drugs. Twenty years ago, the use of drugs that inhibit tumor necrosis factor alpha, known as anti-TNF-ɑ, which were revolutionary, as they work very well and are safe. More recently, there has been an introduction of other antibodies and small molecules against important mediators of inflammation in the gut. Nevertheless, less than 50% of patients show a sustained response to current treatments”.
Salas and her group work to determine which the efficacy of treatments varies between patients, with the goal of understanding Crohn disease and ulcerative colitis. “Studying how the disorder evolves after treatment, whether there is an effect, provides us with highly valuable information on how the disease works”. The idea is to identify new therapeutic targets and biomarkers that predict resistance to the drugs. To reach this goal, the researchers analyze the transcriptome of biopsy tissue. “New technologies such as single-cell RNA sequencing allow us to examine all the genes that are expressed in each of the individual cells that make up the tissue. This leads us to a change in thinking because a single molecule can play different roles depending on the tissue or type of cell where it is expressed. Until now, we have focused on blocking a specific molecule, without taking this complexity into account, and we need to expand our vision to obtain better therapeutic results”.
The researchers also use cells from patients to analyze the interaction between the immune system and the cells that coat the walls of the intestine or to obtain intestinal epithelium organoids. “We work a lot with these cultures in three dimensions, which represent a structure and functions similar to those of the original tissue. Lately, however, we have also been growing cells in two dimensions to study infection with highly adherent strains of the bacterium Escherichia Coli that are associated with Crohn disease and regeneration of epithelial tissue after a lesion”, explains Salas.
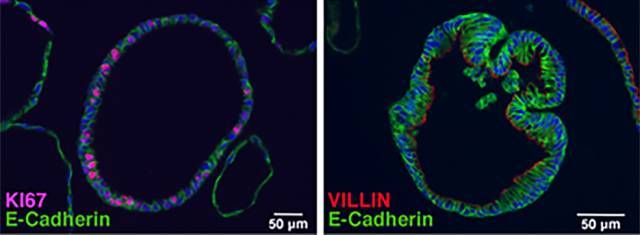
Immunofluorescence image of two intestinal tissue organoids. Membranes (green) and cell nuclei (blue), cytoskeleton (red) and dividing cells (lilac) are observed.
Although most of the group’s studies are carried out using material from patients, researchers have recently completed a project in mice. Specifically, they analyzed the therapeutic potential of nanoparticles that transport interference RNA designed to inhibit an enzyme expressed by cells of the immune system, in a mouse intestinal inflammation model. “The animals presented a disease similar to human ulcerative colitis and our role, as members of the European consortium running the project, consisted of measuring the distribution of the particles and assessing the efficacy of the treatment. It is still in the pre-clinical phase, but this innovative technique may provide a local therapy targeted directly at the inflamed intestine via the gastrointestinal tract”, says the researcher.
Combining clinical practice and research
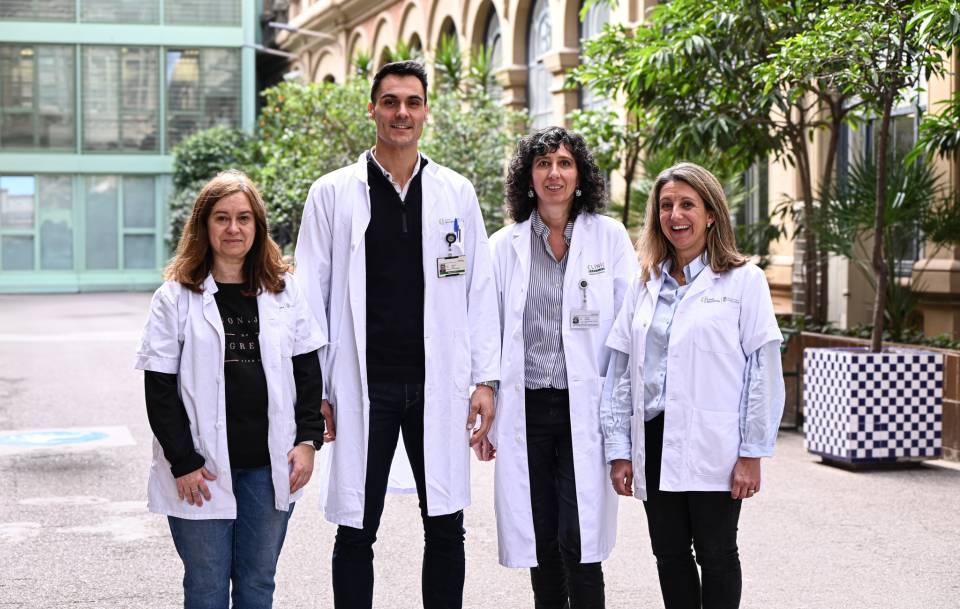
In her group, Salas has clinical researchers who9 focus on the treatment of these patients, the study of new therapies and the development of imaging techniques to study the disease. “Our group is a pioneer in using magnetic resonance indexes of inflammatory activity, particularly in Crohn disease”, states the researcher. These indexes make it possible to evaluate the treatment-sensitive parameters of the tissue that need to be measured to determine the efficacy of the therapy. “It is a very important area because having tools that can detect changes in the tissue will lead to the development of drugs”.
The case of fibrosis, one of the main complications of Crohn disease, where the scarred connective tissue causes occlusions in the intestine, is a good example. There are currently no specific drugs for treating it, but the industry is very interested in designing one. “The problem is that the lack of methodologies for assessing effectiveness limits the ability to conduct clinical trials”, says Salas.
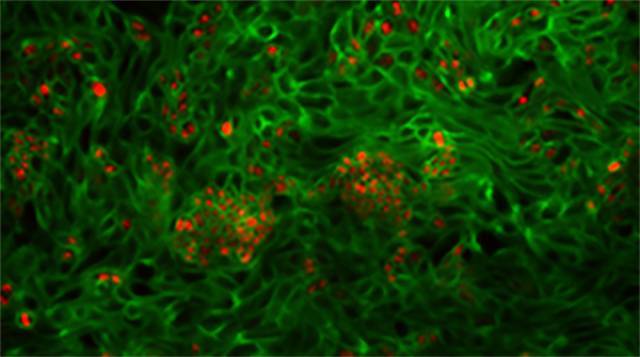
Immunofluorescence image of intestinal cells from patients in culture (green), where proliferating nuclei are also observed (red).
The results of the clinical areas of the group constitute the basis for the recommendations used in the international clinical guidelines. Furthermore, they have made it possible to position magnetic resonance as an alternative assessment and diagnostic technique to colonoscopy. “Our team is highly multidisciplinary, with 50% dedication to research and 50% to clinical practice. This multidisciplinary nature is shown in the research we carry out, which aims to combine both aspects. For instance, in a study currently in progress, we aim to compare data on the gene expression of individual cells with images of perianal fistulas to continue investigating the mechanisms of the diseases and progress toward improving the quality of life of the patients”, concludes the researcher.
This content has been writen with the support of the Spanish Foundation for Science and Technology (FECYT).