The Hospital Clínic de Barcelona-IDIBAPS has developed a new CAR T-cell product, ARI-0002h, and has coordinated a multicentre trial in several Spanish hospitals in order to treat patients with multiple myeloma resistant to the standard treatments. This is the first CAR T-cell product developed in Europe for the disease and its results are encouraging, as all patients improve with treatment and 75% of them maintain their response at 12 months.
Dr. Carlos Fernández de Larrea, haematologist at the Hospital Clínic, Head of the IDIBAPS Mechanisms of progression in monoclonal gammopathies group and coordinator of the clinical trial, presented the results on 12 December at the American Society of Haematology Annual Meeting (Atlanta).
The development of CAR T-cell therapies at the Hospital Clínic has the fundamental support of the "la Caixa" Foundation, thanks to a strategic alliance of 5 million euros to promote pioneering high-impact cancer research and to improve care for cancer patients.
Today, Dr. Josep M. Campistol, Director General of the Hospital Clínic; Dr. Álvaro Urbano-Ispizua, Director of the Hospital Clínic Institute of Haematological and Oncological Diseases; Dr. Manel Juan, Head of the Immunology Service at the Hospital Clínic Biomedical Diagnostic Centre (CDB), of the IDIBAPS Immunogenetics of the autoinflammatory response group and in charge of the joint platforms at the Hospital Sant Joan de Déu and the Blood and Tissue Bank; and Dr. Carlos Fernández de Larrea explained this advance at a press conference.
The trial was carried out in collaboration with the Clínica Universidad de Navarra, which collaborated with the professionals at the Hospital Clínic to produce this type of therapy, and three other Spanish hospitals: the Hospital Clínico Universitario de Salamanca, the Hospital Clínico Universitario Virgen de la Arrixaca in Murcia and the Hospital Universitario Virgen del Rocío in Sevilla. In order to carry out this clinical trial, in addition to support from the “la Caixa” Foundation specific funding was also received from the Carlos III Health Institute (ISCIII) and the Bosch Aymerich Foundation.
Dr. Campistol highlights the fact that, “this is the second CAR T-cell therapy developed at our hospital, which shows the Hospital Clínic’s vocation for research and innovation, focused on providing our patients with the best therapeutic alternatives. CAR-T ARI-0002 is the result of the work carried out by many professionals at the hospital who participated in the various stages of the development of the treatment, from the fine-tuning of the CAR-T to the execution of the trial to demonstrate its efficacy”.
“It is a great satisfaction to see the first results of the Hospital Clínic-CaixaResearch Immunotherapy Unit, which we have supported since its beginnings because it shares our objectives: to be at the side of those who need it most and to improve people’s quality of life. We are particularly proud that this new therapy is aimed at those patients who up to now had no therapeutic alternative. Research shows once again that it is a source of hope and we must continue to support it”, says Àngel Font.
Second CAR T-cell therapy developed by the Hospital Clínic-IDIBAPS
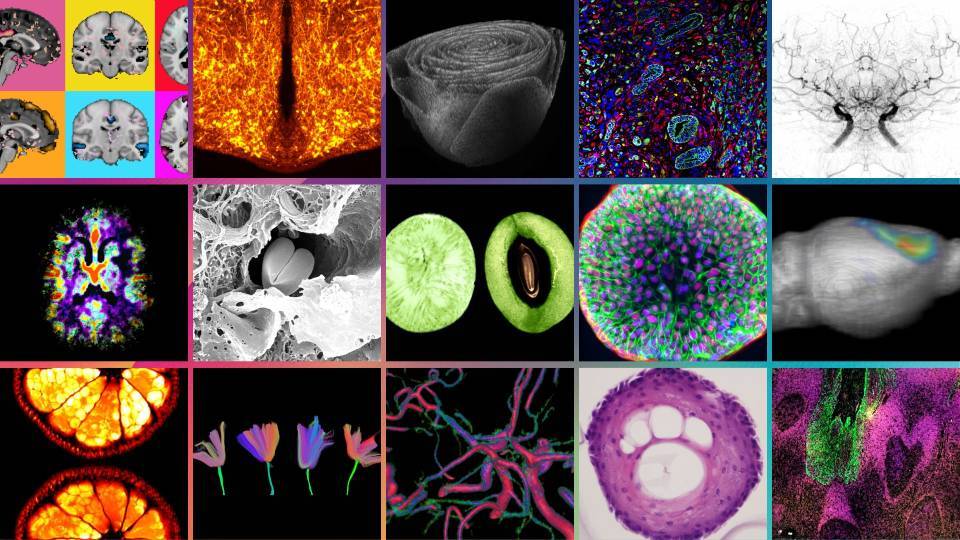
Chimeric Antigen Receptor (CAR) T-cell therapy is a type of cell-based gene therapy in which the patient becomes his/her own donor. It consists of altering the patient’s T cells so that they are able to attack cancer cells. “This is the second CAR T-cell therapy that we have developed at the hospital. On this occasion, unlike ARI-0001 it is directed against another target, BCMA, the most widespread antigen in myeloma immunotherapy", explains Dr. Manel Juan.
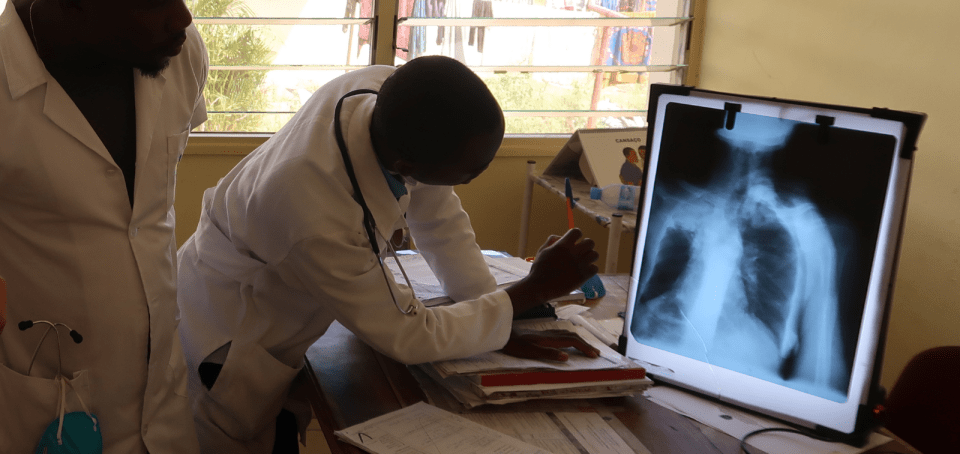
Apheresis, a technique that allows for the separation of the different components of blood, allows T cells to be obtained, a type of white blood cell responsible for the body’s immune response. These T cells are genetically reprogrammed so that, when transfused back into the patient, they can specifically recognize the cancer cells and attack them.
This CAR T-cell therapy targets the BCMA antigen, which is found on the surface of multiple myeloma cancer cells. It was developed by IDIBAPS researchers Beatriz Martín-Antonio, Guillermo Suñé and Lorena Perez-Amill, who demonstrated experimentally in the laboratory that ARI-0002h was very specific and effective against malignant multiple myeloma cells. These results led the AEMPS to approve the clinical trial of ARI-0002h in multiple myeloma patients in whom conventional treatments had failed. “Compared with the previous CAR T-cell therapies that we developed, this one is new and is humanized. Mouse antibodies are often used to develop CAR T-cell therapies and in this case we humanized it in order to ensure it has greater durability in the patient and a lower probability of rejection”, explains Dr. Juan.
Treating patients resistant to multiple myeloma therapies
Multiple myeloma is a type of blood cancer located in the bone marrow where the plasma cells (a type of white blood cell) responsible for producing antibodies that are required to fight off infections are found. In multiple myeloma, the plasma cells undergo an abnormal growth process and form tumours in parts of the bones.
Multiple myeloma accounts for 10% of bone marrow cancers and is the second most common blood cancer, behind lymphoma.
Although there are several treatments for multiple myeloma, ranging from chemotherapy to bone marrow transplantation, some people do not respond and therefore have a very limited life expectancy. The Hospital Clínic-IDIBAPS team has developed a new CAR T-cell therapy product, ARI-0002h, to treat these patients.
The Hospital launched a trial, together with four other hospitals, in order to use ARI-0002h to treat myeloma patients with no other therapeutic alternatives. All the centres carried out apheresis to obtain the patients’ lymphocytes. However, on this occasion professionals from the Hospital Clínic’s Immunotherapy Unit carried out a specific validation at the Clínica Universidad de Navarra so that they could also produce the CAR T-cell therapy and send it to the corresponding hospital.
In addition to the changes in the molecule to target multiple myeloma, “this CAR T-cell therapy is innovative in terms of its administration, and it is divided up into two doses. The first is divided into three small doses to limit toxicity and, after four months, a second dose is administered to the patients in whom the disease has not progressed ”, says Carlos Fernández de Larrea. “This allows us to improve response without significant toxicity”, he adds.
“The results of the trial, in which 30 treatment-resistant patients took part, shows that at 12 months 75% maintain the response and have no disease progression, and 60% have complete remission and no residual disease”, points out Dr. Fernández de Larrea. No neurological toxicity was seen and the immunological adverse effects were mild.
“These results are comparable in efficacy to existing commercial CAR T-cell therapies for multiple myeloma and with lower toxicity”, says Dr. Álvaro Urbano-Ispizua. “Now we are preparing all the documentation based on the results in order to apply to the Spanish Agency of Medicines and Medical Devices (AEMPS) for its use as an advanced therapy drug that was not industrially manufactured”, concludes Dr. Urbano-Ispizua.